Abbreviated breast MRI may expand access to a sensitive screening exam to more women, but for those at average risk of cancer its harms appear to outweigh its benefits, according to a study published July 20 in the Annals of Surgical Oncology.
And although sometimes women with a lifetime of breast cancer risk of less than 20% may be referred to breast MRI in addition to mammography -- perhaps due to having dense tissue, or a palpable mass, or even just because they want reassurance -- the harms of additional screening in the form of breast MRI may be significant, wrote a team led by Dr. Kaitlyn Kennard of Bryn Mawr Hospital in Pennsylvania.
"Abbreviated MRI may introduce average risk women to unnecessary follow-up and increased biopsies with a lower cancer detection rate … [and] should be evaluated closely before implementation."
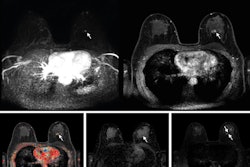
Mammography is the tried-and-true choice for breast cancer screening, but dense tissue diminishes its sensitivity. For women with dense breasts, and for those at higher risk of breast cancer (that is, a greater than 20% lifetime risk), supplemental screening with MRI, ultrasound, or digital breast tomosynthesis (DBT) is often recommended, and MRI is considered by many to be the most sensitive of these modalities.
Yet many women who could benefit from breast MRI refuse it, concerned about long exam times and claustrophobia in the MRI bore.
In part to address these concerns, Dr. Christiane Kuhl of University Hospital Aachen in Germany and colleagues introduced the concept of abbreviated breast MRI in 2013 at the American Society of Clinical Oncology Breast Cancer Symposium. The technique uses a protocol that's designed to retain the benefits of breast MRI without some of the disadvantages of the modality, such as long scan times and impact on workflow.
Since then, the technique has been found useful for women at higher risk, such as those with a prior history of breast cancer. But if it works well for high-risk women, what about everyone else?
After Bryn Mawr Hospital began offering any woman over the age of 30 with any risk profile the option to pay $299 for an abbreviated MRI exam, Kennard and colleagues sought to investigate if the technique is actually effective for women at lower risk.
"Our breast surgical oncology team started this study in response to the implementation of this novel technology in our health system," she told AuntMinnie.com. "Previous studies had looked at abbreviated MRI in women of elevated breast cancer risk but not in low-risk women or women of all breast cancer risk. This provided our team an opportunity to evaluate some of the outcomes for women of average risk undergoing abbreviated breast MRI."
The research included 93 women. Of these, 83.6% had a lifetime risk of breast cancer of less than 20%, but a referring provider recommended abbreviated MRI for the following reasons:
- Presence of dense breast tissue (36.6%)
- Family history of breast cancer (24.7%)
- Palpable mass (12.9%)
Ordering providers were predominately obstetric/gynecology physicians, with breast surgeons following second and primary care physicians third. Of the study cohort, 14% underwent biopsies.
Only one cancer was identified among study participants. Abbreviated MRI led to a change in follow-up screening in just over a third of the women; the most common follow-up protocol was six-month breast MRI (58.6%).
Compared with mammography, abbreviated breast MRI showed high specificity and negative predictive value (NPV), although NPV wasn't statistically significant.
| Abbreviated breast MRI vs. mammography in average-risk women | |||
| Measure | Mammography | Abbreviated breast MRI | p-value |
| Accuracy | 98.6% | 87.1% | < 0.0001 |
| Negative predictive value | 99.8% | 100% | 0.068 |
| Positive predictive value | 35.8% | 7.7% | 0.036 |
Yes, abbreviated MRI has a higher sensitivity when compared to mammography, but among average-risk women it just doesn't seem necessary, the group explained.
"Many women underwent potentially unnecessary biopsies and more aggressive follow-up screening than would otherwise have been recommended, reflecting the low positive predictive value of abbreviated MRI," the team wrote.
So why did these women at lower breast cancer risk agree to undergo abbreviated MRI at all? It's possible that relatively easy access to this imaging technology offers peace of mind, Kennard said.
"One answer is ease of access and lack of need for insurance authorization," she told AuntMinnie.com. "Women were able to pay $299 cash and receive this study. Most of the women did not fit current criteria for breast MRI surveillance, and our [research] brought to light that the use of abbreviated MRI screening for this low-risk cohort may introduce more potential risk over benefits."
The study findings could help other facilities determine the best use of abbreviated MRI in a breast cancer screening program, according to Kennard.
"As other centers evaluate how to implement abbreviated MRI into their breast center, our study may give them pause and the impetus to create institutional guidelines as to who should be candidates for abbreviated MRI," she said.