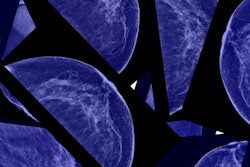
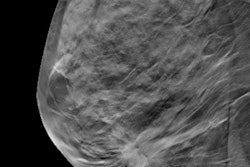
Breast MRI -- along with tests that characterize breast cancer genes -- can help guide treatment for patients with ductal carcinoma in situ (DCIS), according to a study published online January 17 in JAMA Oncology.
The results may address the concerns raised by breast cancer screening critics about overdiagnosis and overtreatment; despite the fact that DCIS is not necessarily a lethal disease, some 70% of women diagnosed with it are treated with surgery, wrote a team led by Dr. Constance Lehman, PhD, of Massachusetts General Hospital in Boston. Whether a woman undergoes radiotherapy after surgery varies widely.
"Advanced imaging techniques, such as breast MRI, may more accurately define the extent of disease, offering the potential to better inform surgical planning," the group wrote. "Tests that involve gene expression profiling may better determine recurrence risk so that radiotherapy can be tailored to those more likely to benefit."
Lehman and colleagues investigated the proportion of patients whose treatment plan for DCIS changed after breast MRI from wide local excision to mastectomy. The group tracked the reasons for the change and also how a test called the 12-gene DCIS score assay guided radiotherapy recommendations. The scoring system estimates 10-year risk of local recurrence based on a scale from 0 to 100, with risk categories defined as low (< 39), intermediate (39-54), and high (≥ 55); women at higher risk tend to be directed to radiotherapy treatment.
The researchers used data from the American College of Radiology Imaging Network (ACRIN) trial E4112, which was conducted between March 2015 and April 2016. Their analysis included 339 women with DCIS who were candidates for wide local excision, each of whom underwent breast MRI before surgery. Pertinent MRI findings were incorporated into the surgical plan. For each woman who had wide local excision as the final surgical procedure (with margins of at least 2 mm), her 12-gene DCIS score was used to guide radiotherapy recommendations.
Of the 339 women eligible for surgery before undergoing breast MRI, 65 (19.2%) converted from wide local excision to mastectomy. For 25 (38.5%) of these women, the change was based on MRI findings. Other reasons for the conversion included patient preference (38.5%), positive margins after surgery (15.4%), positive genetic test results (4.6%), and contraindications for radiotherapy (3.1%).
Of the 171 study participants eligible for radiotherapy due to their DCIS score, 89 women (52%) had intermediate or high scores (≥ 39), Lehman and colleagues found. Of these 171 women, 93% underwent radiotherapy, for a high rate of compliance.
The findings suggest an exciting opportunity for more research, Lehman and colleagues wrote.
"This study may provide useful preliminary information required for designing a planned randomized clinical trial to determine the effect of MRI and DCIS score on surgical management, radiotherapy, overall resource use, and clinical outcomes, with the ultimate goal of achieving greater therapeutic precision," they concluded.