Researchers from the University of Pittsburgh have found that using 1.5-tesla MRI with a continuous arterial spin-labeled (CASL) technique can differentiate with high sensitivity very mild Alzheimer's disease from normal aging.
The study, presented last week during the annual RSNA meeting, concluded that CASL MRI may be a useful screening tool in people who are early in the course of Alzheimer's and is more effective than 1.5-tesla MRI with spoiled gradient echo (SPGR) in detecting potential symptoms.
Alzheimer's and blood flow
Alzheimer's disease is the most common cause of dementia, and reduced regional cerebral blood flow occurs early in the course of the disease when cognitive symptoms are often mild, noted lead author Cyrus Raji, Ph.D., in his presentation.
The study analyzed 32 subjects from the Cardiovascular Health Study-Cognition Study. Nineteen subjects were categorized as cognitively normal controls, while 13 people had a clinical diagnosis of probable Alzheimer's disease using standard research-based criteria.
"Importantly, none of the Alzheimer's subjects in our study had been identified by their primary care physician with dementia, nor were any of them taking any cholinestrerase inhibitors for the cognitive symptoms," Raji said. "Our Alzheimer's subjects were very early in the course of their cognitive symptoms."
Subjects in the control group ranged in age from 76 to 93 years (mean age, 82 years), while the subjects with probable Alzheimer's ranged from 77 to 88 years (mean age, 83 years).
All subjects were imaged with the CASL technique at 1.5-tesla MRI, which provides information on regional cerebral blood flow. SPGR 1.5-tesla MR images were conducted to visualize the subject's hippocampus structure.
Readers' evaluations
Four readers evaluated CASL scans visually to classify them as normal or abnormal based upon the appearance of lower regional cerebral blood flow in regions known to be affected by Alzheimer's disease. The analyses included images of the frontal, temporal, and parietal lobes and the cingulated gyrus.
With SPGR images, visual classification focused on hippocampal atrophy, enlargement of the temporal horns, dilation of the cerebral ventricles, and increase in sulcal width.
The readers then were asked to visually judge each CASL and SPGR scan as normal or abnormal, and rate their diagnostic confidence.
Comparison of the image evaluations to the clinical diagnosis concluded that 1.5-tesla MRI with CASL had greater sensitivity and accuracy than 1.5-tesla MRI with SPGR, but lagged in specificity.
|
In addition, inter-rater reliability was superior in CASL (κ = 0.7 in experienced readers) compared to SPGR (κ = 0.17).
In a review of images, the researchers found imaging characteristics of a false-negative scan to have "patchy perfusion whereby some regions look reasonably well perfused, while some regions, such as the frontal lobes, do not," Raji said. In false-positive reads, the researchers found a reduction in cerebral blood flow throughout the cortex, but not to the same extent as in a true-positive study, or someone with Alzheimer's disease.
"Interestingly, a good number of false positives by CASL [37%] were in people who developed Alzheimer's disease five years later," Raji said. "So, the provocative question is: Were we actually detecting abnormalities prior to the onset of cognitive symptoms? The answer is: I am not sure, because we would need larger numbers of scans over a longer period of time to better understand the finding."
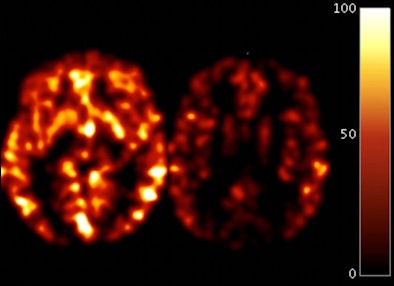 |
| Image shows two axial scans of blood flow with CASL MRI in two individuals. One is from a control subject (left) and one is from a person with Alzheimer's (right). The color bar shows blood flow corresponding to mL of blood per gram of tissue per minute. In Alzheimer's disease, there is reduced blood flow throughout the brain, which occurs early in the disorder. Image courtesy of Cyrus Raji, Ph.D. |
In conclusion, the study found that CASL MRI can be used to separate very mild Alzheimer's from control subjects. "CASL may be a useful tool for detecting mild Alzheimer's disease," Raji added, "but future studies will be needed, comparing it to other perfusion modalities and to use quantitative techniques."
The study was supported by the RSNA R&E Foundation and is scheduled for publication in the May 2010 issue of the American Journal of Neuroradiology.
By Wayne Forrest
AuntMinnie.com staff writer
December 12, 2009
Related Reading
3D software boosts diagnostic accuracy for Alzheimer's, December 1, 2009
Study uses MRI to better detect Alzheimer's, November 17, 2009
ASL-MRI identifies mild cases of Alzheimer's in elderly patients, November 10, 2009
Intense x-rays expose Alzheimer's disease, August 6, 2009
SNM: PET improves dementia diagnoses, June 15, 2009
Copyright © 2009 AuntMinnie.com