Breast MRI is a valuable problem-solving tool in breast imaging, but even this highly sensitive technique can be humbled. Exam timing, indications, and technique are critical to success.
So said Dr. Bruce Porter, medical director of First Hill Diagnostic Imaging in Seattle, who performs two to five breast MRI studies daily, cases that have been referred from throughout the Pacific Northwest.
Presenting his experience at the 2003 National Consortium of Breast Centers conference in Las Vegas, Porter noted that MRI of the breast is beginning to come into its own.
"Only about a half-dozen in the audience are now doing breast MR, but I anticipate that is going to change in the near future," he said. "This is going to become an important tool in your practice."
MRI is just one part of a multimodality approach to breast cancer diagnosis and staging, Porter said. It is appropriate only when a full mammographic and ultrasound evaluation has been performed. Use of high-quality ultrasound is a must as an adjunct for MRI, he said.
The typical breast MRI performed at First Hill begins with a series of T1-weighted images using fat saturation, followed by a bolus of gadolinium contrast and a second series of images acquired over time. Digital subtraction produces a high-contrast image that allows creation of a maximum intensity projection (MIP) image.
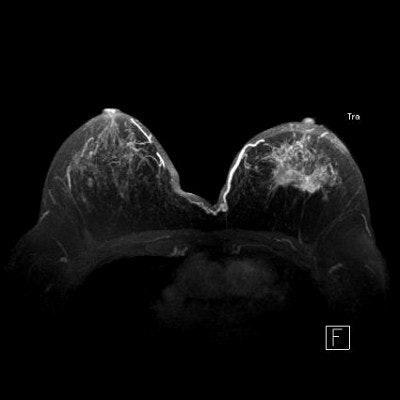
 |
| This 3-D, high-resolution maximum intensity projection (MIP) image illustrates the relationship between tumor and nipple, a key consideration in determining whether lumpectomy or mastectomy is required. Image courtesy of Dr. Bruce Porter, First Hill Diagnostic Imaging. |
The result is a "four-dimensional approach" to imaging, Porter said.
"It’s three dimensions in space, and then the enhancement is tracked through time," he said. "We are not only looking at the morphology of these lesions but also their biology."
Breast MRI is still being standardized, and its accuracy varies considerably with technique. Typical sensitivity ranges between 95%-98%, while specificity roams widely between 38% and 97%. The exam’s negative predictive value is about 95%, while its positive predictive value hovers between 65% and 75%.
Breast MRI excels in several clinical applications. Lobular cancer is a key indication, Porter said, noting studies citing that up to 50% of mammograms in women with lobular cancers can be negative.
Lobular cancer is multifocal or multicentric in nearly one-third of cases, and is also a common cause of positive surgical margins. Due to its diffuse infiltrative nature, it poses multiple diagnostic challenges, Porter said.
"Lobular cancer will humble you most of all," he said. "It is clinically, mammographically, and pathologically a very difficult diagnosis. MR is not infallible but it is very good."
About 30% of the breast MRI cases Porter interprets are lobular cancer, whose spiderweb presentation in the breast and tender tumor tendrils can elude detection.
For lobular cancer diagnosis, Porter relies on a series of MIPs acquired over time to allow gadolinium contrast to leak, pool, and enhance tumor vessels.
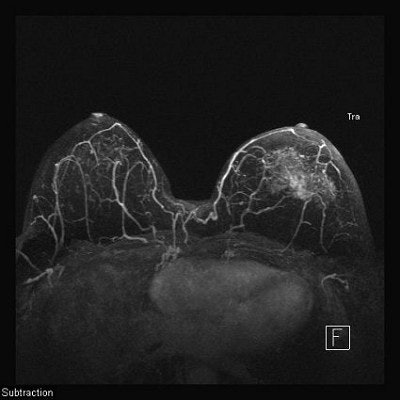 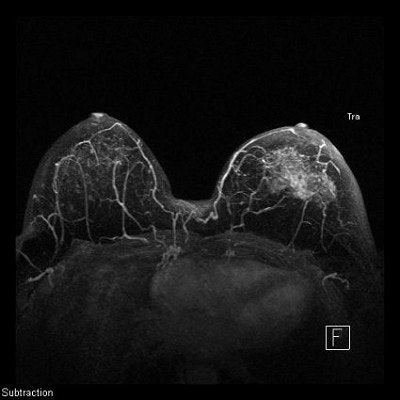 |
The diffuse infiltrative nature of lobular carcinoma makes it difficult to detect. Two-minute (top), four-minute (middle), and thin-MIP (below) views demonstrate contrast enhancement in tumor tendrils over time. Images courtesy of Dr. Bruce Porter, First Hill Diagnostic Imaging.
 |
In breast MRI, timing is everything. Hormonal activity in the breast can wreak havoc, prompting dense tissue to soak up contrast, for example. Porter recommends scheduling breast MRI exams within seven to 10 days after the first day of the patient’s last menstrual period, when breasts are most quiet hormonally.
Another leading indicator for breast MRI includes occult cancer in patients who present with malignant axillary adenopathy but normal breast exam and mammogram. Standard treatment has been mastectomy, but MRI can locate the primary tumor in the majority of cases, allowing breast conservation therapy.
MRI is also useful in evaluating close or positive surgical margins; differentiating from scar versus recurrent tumor; for neo-adjuvant chemotherapy; suspected multiple or bilateral cancers; imaging breast implants; and in high-risk screening of breast cancer gene carriers and patients with prior treatment for lymphoma.
Even within those parameters, breast MRI is not for every freestanding center. With equipment costs starting at $1.2 million, and service contracts averaging 10% of purchase, dedicated breast units are expensive. Exams are time consuming and intensive. Third-party payors may shy from providing reimbursement. Skilled technologists are difficult to find.
"For radiologists, this is not a great way to make a living," Porter said. "It’s a great way to serve the community, but from the perspective of an administrator, it’s nonsensical. I can do two or three knees and read them in the time it takes to do one breast MR. You need to be aware that these are very costly exams."
One way to defray costs is to use an already self-sustaining MRI device with a bilateral breast coil. Use of computer-aided detection (CAD) can also reduce the time required to interpret studies.
Porter is using the CADstream system for breast MRI developed by Kirkland, WA-based Confirma.
"CAD is going to become common for anyone who does a significant volume of breast MRs," he said. "These are complicated cases, and there are technical problems that can make an MR image unreadable. CAD software checks all the parameters to make sure you have an adequate image."
Creating and using a clinical indications list for breast MRI has persuaded third-party payors to reimburse for exams performed at First Hill, Porter said. He recommends that sites develop their own lists and update them frequently, sharing them with insurers to keep them apprised of what MRI can do.
Notably absent from Porter’s own indications list is general breast screening with MRI, a practice he condemns as inappropriate.
"It’s a very bad idea," he said. "The only indications for general screening with MR are breasts and a pocketbook. And having spent the past 12 years developing this as a serious medical tool, I have a real problem with that."
Rely instead on clinical indications that have stood the test of time. MRI’s high negative predictive value translates into high clinical value, Porter said, resulting in high personal value for patients.
"That’s worth quite a lot," he said.
By Deborah R. DakinsAuntMinnie.com contributing writer
March 20, 2003
Related Reading
New adjunctive breast techniques improve positive biopsy rates, February 25, 2003
Mammo plus US negates need for breast MR, December 23, 2002
Post-chemo MRI finds residual tumor in breast cancer, November 14, 2002
Contrast MRI improves cancerous lymph node detection, misses some primary tumors, October 31, 2002
Copyright © 2003 AuntMinnie.com