Combining digital breast tomosynthesis (DBT) and artificial intelligence (AI) could help even more with breast cancer outcomes, but more rigorous trials are needed, according to a presentation given December 1 at the RSNA annual meeting.
In her presentation, Dr. Emily Conant from the University of Pennsylvania talked about opportunities for DBT with help from AI, including improvements in accuracy and efficiency, decreasing variability in image interpretation, and better assessing breast cancer risk.
"I want you just to remember and always think about our patients," Conant said. "What we're really looking for is to improve outcomes for them."
DBT has been available in U.S. markets for 10 years and has been touted by researchers for its higher accuracy over conventional mammography. AI-related research meanwhile has grown over the years for various clinical applications, including breast imaging, as well as aiding radiologists in image acquisition and interpretation.
Conant cited several studies in her talk supporting AI's use in DBT, including some she led.
In one retrospective DBT reader study she led in 2019, she and her team found that readers saw their receiver operating characteristic (ROC) scores improve with the help of AI. Area under the curve (AUC) increased by 5.7%. This includes an 8.4% increase in sensitivity and a 6.9% in specificity. Recall rate and reading time also decreased by 7.2% and 52.7%, respectively. However, no false negatives were included in the study.
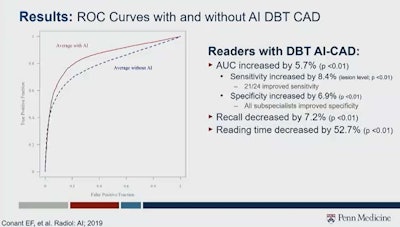 Combining artificial intelligence with digital breast tomosynthesis has shown promise when used alongside radiologists or by itself. One study led by Dr. Emily Conant, who gave a keynote speech at the RSNA annual meeting on this topic, found that area under the curve, specificity, and sensitivity increased when using this combined method, while recall rate and reading time decreased. However, Conant said more rigorous, prospective clinical trials, among other things, are needed. Image courtesy of Dr. Emily Conant.
Combining artificial intelligence with digital breast tomosynthesis has shown promise when used alongside radiologists or by itself. One study led by Dr. Emily Conant, who gave a keynote speech at the RSNA annual meeting on this topic, found that area under the curve, specificity, and sensitivity increased when using this combined method, while recall rate and reading time decreased. However, Conant said more rigorous, prospective clinical trials, among other things, are needed. Image courtesy of Dr. Emily Conant.Another reader study Conant cited was published in 2021, with the researchers finding that AUC, sensitivity, and specificity increased for readers with the help of AI when it came to single-view, wide-angle DBT. While reading times remained unchanged, standalone AI had an AUC higher than the average reader (0.90 vs. 0.85).
For triaging, Conant said AI with DBT can help with workforce shortages. The results of one study she cited from 2021 indicated that AI helps DBT double reading by decreasing its workload by 72.4% and decreasing the recall rate from 4.4% to 3.7%. For single reading, workload was also decreased by 72.4%.
Conant also led a study presented at the 2021 European Congress of Radiology in which the researchers found DBT-AI triaging at a 0% false-negative rate identifies 33.4% of screening exams. The team also found that by combining case scores with age and density, triaging could potentially increase to 58.6%.
For risk assessment, DBT with AI has also shown promise. The authors of one European study published in 2020 that Conant cited found that AUC increased when adding factors such as lifestyle and familial risk, as well as polygenic risk score, to a two-year risk AI model. The values were significantly higher than using polygenic risk scores or the Tyrer-Cuzick model alone.
So, what's next? "Lots of steps," Conant said.
These include rigorous, prospective clinical trials with larger, diverse populations and clear outcomes, as well as cancer localization.
"We need transparency in algorithms and collaboration across multiple sites, so we can really improve the generalizability of these algorithms," Conant said. "And we need standardization of outcomes."
Conant also said safety and regulations should be looked at when considering the legal and ethical ramifications of using this combined imaging method.