Breast cancer remains the most commonly diagnosed cancer among women in the U.S.i Thankfully, the field of breast screening is not static, and advancements are revolutionizing how we detect and diagnose the disease.
 Erik Anderson, president, breast & skeletal health solutions at Hologic.
Erik Anderson, president, breast & skeletal health solutions at Hologic.
While recent breakthroughs have improved our understanding of breast cancer and addressed many challenges, there's vast potential for future improvements to make screening even more effective. By implementing existing technologies more broadly and exploring new approaches, we can create a screening experience that is both more accurate and accessible for all women, paving the way for earlier breast cancer detection.
Understanding breast density
Recent updates to the U.S. Food and Drug Administration’s (FDA) Mammography Quality Standards Act (MQSA) mandate that clinicians inform patients about their breast density, elevating reporting requirements and the FDA’s auditing capabilities for consistent, high-quality care nationally.ii These new guidelines bring breast density to the forefront of discussions in women's health. Fortunately, technology advancements have better-equipped health systems to screen and diagnose patients with dense breast tissue, offering a plethora of options to best meet a patient’s unique needs.
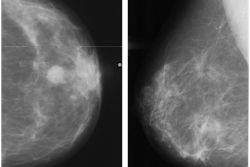
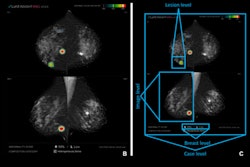
In screening programs, digital breast tomosynthesis (DBT) has distinguished itself in recent years as offering a clearer view that finds more cancers than 2D mammography, including for women with dense breasts.iii The technology has been adopted by 87% of FDA-certified mammography facilities in the U.S.,iv making it a more accessible option than ever before. New AI integrations are further elevating the impact of this technology, not only by acting as a valuable second set of eyes for radiologists but also by providing standardized breast density assessments.
For dense-breasted patients requiring supplemental imaging, MRI remains a valuable option that is not limited by breast density and is shown to be more sensitive than mammography at finding breast cancer.v More recently, contrast-enhanced mammography (CEM) has emerged as an accessible diagnostic alternative with comparable imaging benefits to MRI, while also offering time savings and increased accessibility to a broader community.vi Investigations continue of this newer imaging modality, which has the potential to positively benefit patients with dense breasts.
Ultrasound rounds out the radiologist’s toolkit for supplemental imaging of women with dense breasts. Both handheld and automated ultrasound methods are shown to be effective in detecting mammographically occult cancer in women with dense breast tissue. Research demonstrates that ultrasound substantially enhances the detection of clinically significant, small, mostly invasive, and node-negative cancers.vii Moreover, automated breast ultrasound (ABUS) tends to be increasingly used as a supplementary technique in the evaluation of patients with dense glandular breasts.
Advancements in technology are continuously raising the bar for early detection. The future of breast density assessment lies in seamlessly integrating these advancements into the standard screening regimen and expanding access to the latest technologies. Leveraging these advancements alongside AI integrations paves the way for precision medicine in breast cancer screening where we can tailor care based on the individual needs of the patient for improved health outcomes. By combining advanced breast screening tools, we can create a more comprehensive approach so that every patient benefits from the advantages offered by the latest technologies.
Improving accessibility, equity
There is growing recognition that we must rectify longstanding disparities in accessibility and equity within breast cancer screening. This involves establishing equitable access to high-quality screening services tailored to the diverse needs of all women. Experts are increasingly calling for more diverse datasets to train the AI algorithms used in breast screening.viii This ensures accurate training information for women of all backgrounds, fostering inclusivity in algorithm development.
Looking ahead, there's a pressing need to bridge the gap by providing screenings that advance not just technologically but also in terms of cultural and linguistic accessibility. For example, by incorporating robust multi-lingual capabilities as standard features in screening technologies, providers can effectively meet their patients where they are.
Inclusivity extends beyond language barriers to patients with physical limitations, such as those who use wheelchairs or encounter positioning challenges during screening, including frozen shoulder or kyphosis (curvature of the spine). A large population of individuals in the U.S. grapples with various disabilities, with 13.6% of women over the age of 18 facing mobility challenges.ix
These challenges can make accessing healthcare difficult and impact screening compliance, especially when some imaging technology isn’t made with these mobility challenges in mind. Women ages 50-74 with disabilities are 50% less likely to undergo mammography screening compared to non-disabled women.x
Ensuring we reach these women is of utmost importance, given the critical nature of mammography screening. If we can optimize our technology to meet women where they are, we have the opportunity to rectify this situation and attract more women to undergo screening. Innovation should consider the needs of every patient, including those with special needs, to create a truly inclusive screening experience.
One key advantage of AI is its ability to democratize access to high-quality breast cancer screening. In remote or underserved areas where finding a radiologist specializing in breast imaging can be challenging, AI can act as a powerful equalizer. AI can enhance the capabilities of local radiologists who may have broader imaging expertise, potentially leveling up their abilities to match the accuracy of specialists.
That way patients in these communities receive high-quality screening and potentially life-saving diagnoses, regardless of their location. Point-of-care AI can also empower health facilities to better cater to the needs of patients from remote locations by prioritizing real-time reading of screening cases for patients facing significant travel distances, thereby reducing the need for burdensome return visits that could impact patient compliance. Embracing ongoing advancements can contribute to the recent progress, ensuring that breast cancer screening technology evolves to be more inclusive for individuals of diverse backgrounds.
Enhancing image quality
The goal of screening is clear, aiming to accurately identify breast cancer in patients every time. The advent of AI-powered tools is further revolutionizing breast cancer detection, as they can analyze mammograms with remarkable accuracy, potentially identifying lesions highly likely to be cancerous. As the technology matures and algorithms are further refined, radiologists are gaining greater confidence in the specificity of results. Some newer AI tools can save radiologists valuable time by quickly navigating to relevant areas on the images, eliminating the need to manually search for potential correlations.
The highest image quality can only go so far if the patient is not accurately positioned to capture the complete view of the required breast tissue. This can waste valuable time. By analyzing key metrics such as patient positioning and compression techniques, these platforms can help merit consistent quality and reduce the need for retakes due to technical errors. Today's AI-backed point-of-care analytic integrations not only track key performance metrics but also narrow in on positioning and compression techniques. This capability empowers centers to identify and address positioning issues among technicians proactively, preventing potential time-wasting problems and the need for frequent retakes.
Despite the recent advancements, today’s current tools still exhibit opportunities to improve clinical outcomes individualized to all patients, highlighting the need for ongoing innovation to address this unacceptable gap. Improving image quality is a top priority, enabling more accurate breast cancer detection and driving a relentless pursuit of enhanced screening methodologies.
Addressing staffing shortages, burnout
In today's healthcare environment, radiologists are facing increased demands and taking on more responsibilities. A global shortagexi of radiologists and growing imaging volumesxii contribute to this strain, causing radiologists to report a surge in burnout rates, recently reaching an alarming 54%.xiii Embracing the latest advancements can streamline workflow and enhance the effectiveness and efficiency of radiologists, helping to ease the workload burdens they face.
Modern AI software can play a pivotal role in optimizing workflows by enabling radiologists to prioritize cases using computer-aided detection (CAD) markings. Additionally, AI can automatically generate lesion correlation markings across different views, potentially reducing the time spent searching for correlated lesions. These innovations offer valuable solutions for radiologists contending with staffing shortages, heavy workloads, and the challenges posed by today's healthcare system.
A shift toward remote work is increasingly becoming recognized as a valuable solution to address staffing shortages and combat burnout among radiologists. Thanks to recent advancements in workstations and IT workflow platforms, health systems now possess the potential to establish at-home reading environments, enabling radiologists to make informed decisions by analyzing breast studies from the comfort of their homes. This flexible arrangement can not only enhance focus and productivity but also serve as a promising approach contributing to the overall well-being of radiologists.
This trend in burnout extends beyond radiologists and encompasses technologists as well, constituting an ongoing problem within the field. One solution is to involve technologists in the decision-making process, empowering them to contribute to strategic choices that directly impact their workflow. Implementing technology that utilizes data to drive point-of-care decision-making is equally essential, fostering reproducibility in processes and outcomes, irrespective of technologists' tenure.
Breast cancer screening protocols will evolve with ongoing research and data, involving reassessment of criteria and exploration of innovative prioritization methods using advanced technology. The integration of AI is set to enhance radiologists' roles, granting them more control over their workday to focus on delivering excellent patient care.
Conclusion
The latest advancements in breast screening encompass a diverse spectrum, including new technologies, treatment innovations, and screening advancements, all significantly contributing to positive outcomes. Notably, the mortality rate for U.S. women with breast cancer has seen a remarkable 58% decrease from 1975 to 2019.xiv
While this progress is commendable, it serves as a poignant reminder that further innovation is imperative. We must explore developments that deepen our understanding of breast density as a risk factor, build on existing strides in accessibility and inclusivity, refine image quality, and better address the needs of overworked and understaffed radiology departments.
Erik Anderson is president, breast & skeletal health solutions at Hologic.
The comments and observations expressed are those of the author and do not necessarily reflect the opinions of AuntMinnie.com.
iii https://pubs.rsna.org/doi/10.1148/radiol.221571
v https://www.breastcancer.org/research-news/fast-mri-better-than-3d-mammo-for-dense-breasts
vi https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7997616/
vii https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5872003/
viii https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10625863/
x https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4628215/
xi Konstantinidis K. The shortage of radiographers: A global crisis in healthcare. J Med Imaging Radiat Sci. 2023 Oct 19:S1939-8654(23)01877-5. doi: 10.1016/j.jmir.2023.10.001. Epub ahead of print. PMID: 37865586.
xii Poyiadji N, Beauchamp N 3rd, Myers DT, Krupp S, Griffith B. Diagnostic Imaging Utilization in the Emergency Department: Recent Trends in Volume and Radiology Work Relative Value Units. J Am Coll Radiol. 2023 Dec;20(12):1207-1214. doi: 10.1016/j.jacr.2023.06.033. Epub 2023 Aug 4. PMID: 37543154.
xiii Kane, L. US physician burnout & depression report 2023. Medscape. January 27, 2023. Accessed February 16, 2024. https://www.medscape.com/slideshow/2023-lifestyle-burnout-6016058?faf=1
xiv Caswell-Jin JL, Sun LP, Munoz D, et al. Analysis of Breast Cancer Mortality in the US—1975 to 2019. JAMA. 2024;331(3):233–241. doi:10.1001/jama.2023.25881