CHICAGO -- When AI in mammography is coupled with a safeguard radiologist review, women are more likely to pay for breast cancer screening mammography if the AI will boost exam results, research presented December 5 at the RSNA meeting suggests.
The finding comes from a study of nearly 750,000 women who chose to enroll in a self-pay, AI-enhanced breast cancer screening program. The research enrolled women across 10 clinical practices, ranging from a few sites up to 64 sites at the largest practice.
Investigators explored the impact of adding AI to mammogram screening exams. For those enrolled, the clinical practices applied a U.S. Food and Drug Administration-compliant AI software to their mammograms. An expert breast radiologist also provided a third, "safeguard review" in cases where there was discordance between the first reviewer and the AI.
“This is the first report on results from a program that provides an AI-powered enhanced review that patients can elect to enroll in,” said study lead author Bryan Haslam, PhD, from RadNet subsidiary DeepHealth in Somerville, MA, in an RSNA statement.
Out of the 747,604 women who underwent screening mammography over an initial 12-month period, the overall cancer detection rate (CDR) was on average 43% higher for enrolled women than for unenrolled women, according to the findings.
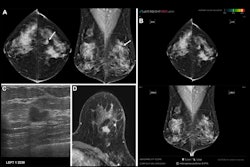
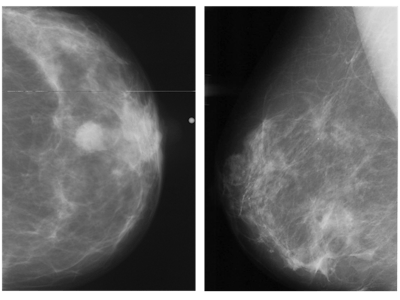 Abnormal mammogram (left) compared with normal mammogram. Image courtesy of the RSNA.
Abnormal mammogram (left) compared with normal mammogram. Image courtesy of the RSNA.
All 10 practices saw a substantially higher CDR in enrolled women compared with unenrolled women. Of the overall CDR, researchers further noted a 21% increase in cancer detection that they attributed to the AI program. They credited the remaining 22% increase in cancer detection to the fact that higher-risk patients chose to enroll more frequently.
“The AI-driven enhanced review program leverages AI in a novel workflow to ensure women with suspicious findings get expert-level care that could help detect many more breast cancers early," Haslam added. "The number of women electing for this program is now at 36% and growing, and the rate of cancer detection continues to be substantially higher for those women.”
Cancer detection rate, recall rate, and positive predictive value (PPV1) were calculated per practice using routine Mammography Quality Standards Act methodology, the study noted. Overall, the recall rate was 21% higher for enrolled versus unenrolled women at 10.9% versus 8.8%, and the PPV1 was 15% higher at 5.4% versus 4.6%.
Data indicate that many women are eager to utilize AI to enhance their screening mammograms, the study's senior author, DeepHealth CEO Gregory Sorensen, MD, added. "When AI is coupled with a safeguard review, more cancers are found,” he said.
The study is important because self-pay programs may offer a way for patients to get access to AI-enhanced screening care that could result in more cancers detected early. Combining an AI program with patient self-selection merits further research, the researchers concluded.
For full 2024 RSNA coverage, visit our RADCast.