Areas in Canada that offered annual mammography screening to women with dense breast tissue saw lower rates of interval breast cancers compared with locations that offered biennial screening, according to a study published July 19 in the Canadian Association of Radiologists' Journal.
A team of researchers examined data on 148,575 women with dense breasts screened between 2008 and 2010, according to lead author Dr. Jean Seely, a professor of radiology at the University of Ottawa in Ottawa in Ontario, Canada. Seely is also president of the Canadian Society of Breast Imaging.
The team found a total of 288 invasive interval breast cancers -- defined as breast cancers detected during the interval after a normal screening mammogram and before the next screen is due. The group then analyzed the data in the following two ways:
- By programs that set screening intervals based on routine policy, with women with dense breasts getting annual screening.
- By programs that offered biennial screening intervals for all women, but radiologists could override local policy and order annual screening for women with dense breasts.
Programs that offered annual screening for women with dense breasts resulted in a lower interval cancer rate (ICR) compared with those that offered biennial screening, a result that was statistically significant. Programs that offered screening based on radiologist recommendation saw an even bigger difference, but the difference was not statistically significant.
| Interval breast cancers by mammography screening interval | ||||
| Annual screening | Biennial screening | Percent difference | p value | |
| Interval breast cancer rate for programs based on routine policy | 0.89 cancers/1,000 women | 1.45 cancers/1,000 women | 63% | p = 0.0016 |
| Interval breast cancer rate for programs offering screening on radiologist recommendation | 0.93 cancers/1,000 women | 1.7 cancers per 1,000 women | 83% | p = 0.0605 |
Seely and colleagues also found that in screening programs where radiologists' screening recommendations were able to be analyzed, a total of 76,103 women were screened, with 87 interval cancers detected.
The data was sourced from the Canadian Breast Cancer Screening Database, which is operated and maintained by the Public Health Agency of Canada on behalf of the Canadian Breast Cancer Screening Network, Seely noted.
"The dense breast tissue masks the cancer. It can be masked on all mammograms," Seely said in an interview with AuntMinnie.com. "If we do more regular screening, we are likely to pick up a tumor on an annual screen, rather than wait two years."
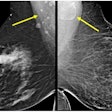
Seely pointed out that more than half of the mammograms in the sample (57%) were performed with film, which is no longer used, as all mammograms in Canada are currently performed with digital mammography.
"It [mammography] has definitely improved and that [digital mammography] would improve the breast cancer detection rate," Seely said, citing research suggesting that digital mammography improves cancer detection by 20% in women with dense breasts.
Still, flat-panel digital mammography was used in 22% of mammograms in the study, while computed radiography mammography was used in 21% of mammograms, suggesting these modalities also missed cancers, noted Dr. Seely.
The findings underline the need for annual screening for Canadian women who are categorized as BI-RADS D in their breast density, Seely said. In addition, there should be mandatory notification to Canadian women about their breast density if they are categorized as BI-RADS D, she believes.
"This is a huge impetus for breast dense notification in Canada," Seely said. "Women want to know if they have this risk factor. In the past, they may have been falsely reassured by a normal mammogram and go on to have a worse outcome for breast cancer than women with nondense breast tissue."
Specifically, women with breast density categorized as BI-RADS D have a much greater risk of breast cancer, poorer outcomes, and greater risk of mortality due to breast cancer compared with women who are not in the BI-RADS D category, Seely said.
A limitation of the study is that it did not capture data from all jurisdictions in Canada, according to Seely, focusing on Newfoundland and Labrador, Ontario, Quebec, Manitoba, and New Brunswick, as well as the Northwest Territories, which together represent about two-thirds of the country's population. Jurisdictions that were missing included Alberta, British Columbia, Nova Scotia, Prince Edward Island, Saskatchewan, and Yukon.
Supplemental screening, such as using ultrasound or MRI, may help reduce the rates of interval cancers in women with dense breasts, Seely noted, and it could be considered in the future in breast cancer screening programs in Canada.
"We know we need more than just mammography," Seely concluded.