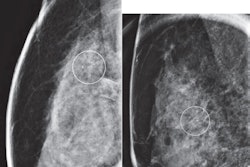
Detecting breast arterial calcifications on routine mammograms could identify women at a higher risk of future cardiovascular disease (CVD), a study published March 13 in Clinical Imaging found.
Researchers led by Shadi Azam, PhD, from Weill Cornell Medicine in New York found links between such calcifications and older age, diabetes, parity, younger age at first birth, and hypertension in women who underwent both screening mammography and cardiac CT angiography (CCTA).
“Additionally, we found that when neither breast arterial calcifications nor coronary arterial calcifications were present, the estimated 10-year risk of developing atherosclerotic CVD was lowest, whereas the highest risk was observed when both [calcifications] were present,” Azam and colleagues wrote.
Breast arterial calcifications are incidental findings on mammograms. While previous studies have suggested an association between these findings and cardiovascular diseases, questions remain about the clinical utility of reporting them and managing of women who have these calcifications on mammography.
The Azam team studied lifestyle, reproductive, and cardiovascular determinants of breast arterial calcifications in women undergoing mammography screening. It also estimated 10-year atherosclerotic CVD risk via associations to breast and coronary arterial calcifications.
The researchers collected data from 215 women aged 18 or older who underwent mammography and CCTA within a two-year period between 2007 and 2017. They categorized breast arterial calcifications as binary (present/absent) and semi-quantitatively (mild, moderate, severe). Meanwhile, coronary arterial calcifications were recorded as binary (present/absent).
Of the total women, 38 (18%) had breast arterial calcifications found on mammography. The team reported that several patient characteristics are tied to these calcifications.
| Associations between breast arterial calcifications and patient characteristics (odds ratios, with 1 as reference) | ||||
|---|---|---|---|---|
| Crude | p-value | Age-adjusted | p-value | |
| Older age (60 years and older) | 5.77 | 0.0002 | N/A | N/A |
| Presence of diabetes | 2.77 | 0.02 | 2.54 | 0.06 |
| Parity | 4 | 0.006 | 3.31 | 0.02 |
| Younger age at first birth (28 years and younger) | 3.11 | 0.009 | 2.73 | 0.03 |
| Blood pressure of 80 or greater (diastolic) | 1.95 | 0.05 | 2.45 | 0.03 |
| Blood pressure of 130 or greater (systolic) | 4.33 | 0.0002 | 3.21 | 0.005 |
| Presence of hypertension | 2.04 | 0.05 | 1.45 | 0.35 |
The following characteristics did not have significant associations with breast arterial calcifications: High body mass index (BMI), hyperlipidemia, inflammatory or autoimmune disease, smoking status, or family history of cancer (crude), previous breast biopsy, estrogen hormone therapy, age at menarche, and oral contraceptive use.
Also, women with both breast and coronary arterial calcifications had the highest estimated 10-year risk of atherosclerotic CVD risk at 13.3%. Women with only breast arterial calcifications had an estimated risk of 8.8%; those with only coronary arterial calcifications had a risk of 5.8%; and those with neither calcification had a 4.4% risk.
Finally, the team reported no association was detected between the presence of breast and coronary arterial calcifications.
The study authors highlighted that finding links between the mammographic presence of breast arterial calcifications and CVD risk could help better manage patients without the need for additional exposure to radiation and could help save on costs.
“Further research in large cohorts with longer follow-up period is needed to better delineate the association between [calcification] burden and CVD outcomes and to establish the clinical utility of reporting breast arterial calcifications detected through mammography screening,” they added.
The full study can be found here.