
AuntMinnie.com presents the 19th in a series of columns on the practice of ultrasound from Dr. Jason Birnholz, one of the pioneers of the modality.
Everyone in the world knows by this time that the RSNA meeting is coming -- or, at least, everyone in medical imaging. I've attended more than 40 of these annual meetings, and I'm very proud that I have presented one or more scientific papers at 37 or 38 of them myself.
 Dr. Jason Birnholz.
Dr. Jason Birnholz.The first meeting I remember was held at the Bismarck Hotel in Chicago in 1971, when I was a second-year resident in diagnostic radiology. There wasn't a big manufacturer presence onsite, but most of the big film companies and x-ray equipment manufacturers took lots of attendees out to extravagant dinners, including house staff and technologists. I always wanted to thank those reps for their acts of kindness that are surprisingly reaffirming at the start of one's career. Oh well, commercial civility is not that prevalent nowadays.
In 1971, and I presume at most previous RSNA meetings, there was a respectful balance between the private-practice radiologist majority and the academic radiologist minority. The two communities seemed close and collegial. However, the RSNA meetings of recent years seem to have been dominated by the academic side, and there has been an increasing presence of scientific presentations by resident physicians and subspecialty fellows from larger departments, almost like a requirement in current postgraduate education programs.
A lot of the scientific presentations in those halcyon days of yore were observational research, which is traditional and well-suited to clinical imaging. I have been sensing, though, for the past two decades that RSNA has been seeking to improve the apparent scientific rigor of the program by encouraging papers using analytic techniques of bench research that are not entirely well-suited to the subject matter. There has also been a progressive increase in econometric analyses, even though these are often invalidated by technical advances in the interim between data collection and presentation.
RSNA is about radiology in all its forms. In the early 1970s, when imaging modalities were so much more limited, there was no identification of a distinct "ultrasound" category. This later administrative development was a highpoint in the 1980s through the mid-1990s, as our subspecialty really began to flourish.
I find it interesting that lately the unique identity of ultrasound is being erased as it is merged into systemic or regional topic areas with every other imaging method. RSNA never had much interest in cardiac ultrasound that I can recall, and there is now only a remnant of the obstetrical ultrasound presence of 20 years ago.
Actually, that trend does not bother me at all. I'm confident in my abilities in ultrasound, and I always learn the most at scientific meetings from papers on everything else nonultrasound. However, I am saddened that radiologists in training today will not have the interest or educational background to continue vigorously advancing ultrasound, especially when we seem to be on the brink of some major technical advances.
The basic common denominator
The basic common denominator of the RSNA meeting is "images." When we visit the booth of a manufacturer, we judge the value to our practices from the clinical and phantom images that we see.
There is information about how easy or hard it is to generate similar images and the technique used that is better suited to word of mouth, but this is really of secondary importance to the experienced operator. The problem is that manufacturers want to illustrate performance features of their equipment, and the selection of such images rarely reflects what interpreters regard as significant, striking, or necessary for everyday work.
I'm going to provide an annotated example, because there is something basic that every radiologist knows but that I find difficult to express verbally. The notion is that good images talk to you, and at a profound level that may not even be conscious, where one synthesizes imaging appearances and image quality with prior knowledge and extant clinical information into a tentative diagnosis.
 A 2D sector image from a routine exam at 19-weeks gestational age. Image courtesy of Dr. Jason Birnholz.
A 2D sector image from a routine exam at 19-weeks gestational age. Image courtesy of Dr. Jason Birnholz.A common reaction to this image would be that there's nothing impressive about it, let alone that it might be worthy of featuring. Boring, next case, is it break time yet? The image above is an original, direct from the machine, with cropping but no additional postscan processing. It's about 5 years old, and its main technical flaw is lateral resolution spreading, which was really typical of beamformers and smaller-aperture arrays at the time. The markers atop the image are at 5-mm intervals.
There's not much noise in the image. There is flow streaming from platelet clumping and red cell rouleaux in the umbilical vein. The speckles in the amniotic fluid are real, being clumps of flaked-off skin and clear meconium.
This is actually a really good sign in second-trimester exams that you would miss in an image that incorrectly shows amniotic fluid as clear. Amniotic fluid is complex, like everything else in biology. An excellent review can be found in a 2005 article by Dr. Mark Underwood, Dr. William Gilbert, and Dr. Michael Sherman (Journal of Perinatology, May 2005, Vol. 25:4, pp. 341-348).
In medical imaging, picture aesthetics are always balanced by what you know about the target, like the normal and expected presence of meconium in the second trimester as a sign of well-being. This is the difference between the casual image viewer and the interpreter.
The central feature is a portion of the umbilical cord. It doesn't even seem to be a "good picture of the cord," which is most often depicted in 2D images as a simple cross section showing the big vessels. What it does show very well is a good amount of Wharton's jelly. Does that really have any meaning?
The limitations of an unquestioned verbal 'definition'
I am digressing to mention the Whorf hypothesis, named for Benjamin Whorf, a 1918 chemical engineering graduate of the Massachusetts Institute of Technology (MIT), not the noted Klingon security officer. Whorf's passion and hobby was linguistics when the field was new, and he collaborated and studied with some of the founders of that discipline at Yale University while he was working as a fire inspector for a Hartford insurance company.
Based on his experiences in the Southwest with Indian languages having no ancestral relationship to Western European languages, he came to a conclusion that went something like this: What you think depends on the language you are thinking in.
An example was how arcane and novel special and general theories of relativity could seem to Western European language speakers (in the 1920s/1930s), while seeming to be an integral part of the world view of the Native American Indian speaker. The Whorf hypothesis resurfaced in the 1960s with the notion of the difficulties of the Western diplomat conversing and thinking in a dyadic, black-or-white, judgmental language when communicating with his or her Chinese opposite, who is conditioned to nuances and many shades of gray between any extremes. There were also some bold attempts to develop psycholinguistics as a way to infer processes of disordered thinking from observed patterns or slips in speech or written language.
I understand that the Whorf hypothesis, or "linguistic relativity," has been discredited completely for some years, or at least relegated to the "wrong, but good try" bin. Psycholinguistics does not seem to have had much traction either.
However, it seems to me that there is something Whorfian in the way we treat something because of its name or common definition. Take the chicken and the egg paradox. If a chicken is a creature that lays a calcium-shelled ovoid egg, and an egg is defined just as a calcium-rimmed ovoid thing produced by a chicken, then you have the fun, endless regression paradox that's amusing and insoluble.
If you take a specific biological definition of a chicken and a general definition of an egg, then the ancestor laying the egg that bore the first proto-chicken was something else in a biological sense.
The disembodied umbilical cord
Most of us have had a notion of the umbilical cord as a passive conduit conveying blood between the fetus and its placenta, or as the passive tubular part of the fetal "supply line." The important parts are the vessels, and the forms of pathology we seek for cords -- visually or by Doppler -- emphasize blood flow diminished by compression, constriction, twisting, knotting, and the like, as well as the factors that may impair the structural integrity of the cord and increase its vulnerability to compression.
The clinical consequence can be instant, massive, and lethal, or small and chronically repetitive, relieved by compensatory mechanisms diminishing oxygen debt to critical organs. There is also the traditional practice of discarding the cord after delivery as medical waste, so how important could it ever be?
Clinical ultrasound researchers are good observers. Going back a few years, when images tended to be noisier, there were several excellent works that noted that cords tended to be very "thin" or "lean" with growth retardation. There were even a few such as this paper (Ultrasound in Obstetrics and Gynecology, March 1999, Vol. 13:3, pp. 176-80) that went the other way, i.e., "Gee, that cord is really thick in this macrosomic, LGA fetus." All true.
Thinking of the cord as a passive conduit leads to regarding changes to the substance of the cord as late and secondary signs of something else, like protein loss with intrauterine growth restriction (IUGR) or maybe increased water content with macrosomia.
Regenerative medicine
There is another explanation suggested by the marvelous new field of regenerative medicine, in which stem cells are used to reprogram or replace injured cell lines. Public or private cord blood banking is now recommended for all deliveries, which is based on more than 20 years of using hematopoietic stem cells in the treatment of childhood leukemias and an ever-increasing spectrum of other pediatric conditions spanning neoplastic to immune and inflammatory. Those same recommendations include a request that a segment of the umbilical cord also be preserved.
The umbilical cord is a rich source of mesenchymal stem cells (MSCs), which have some remarkable properties. MSCs do not require the same degree of histocompatibility that is essential for therapeutic use of hematopoietic stem cells, nor do they seem to require the continuous use of immunosuppression after treatment.
MSCs transform into ectoderm-derived cells like skin, nerve, and muscle; replacing damaged myocardium is a great emerging application. Very recent work suggests that in utero MSCs have a big but largely unknown role in the development of immune competences.
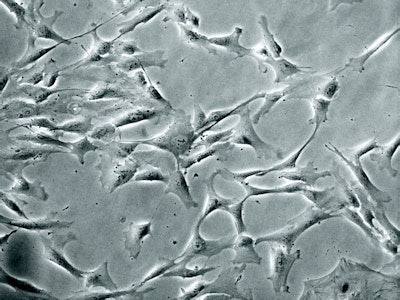 Mesenchymal stem cells from an umbilical cord segment. Courtesy of Prof. John Davies, www.verypowerfulbiology.com.
Mesenchymal stem cells from an umbilical cord segment. Courtesy of Prof. John Davies, www.verypowerfulbiology.com.As a general rule in the complex world of biology, everything has a function. And, there is both redundancy and multifunctionality. Maybe the right way to think of the cord is as a conduit for blood with some other major function, like the continuous production and circulation of mesenchymal stem cells both ways in the umbilical cord and into amniotic fluid.
In this light, fetal growth retardation, which results from inflammation and then sclerosis of small vessels in the placenta, might very well be due to the lack of MSCs to the placenta. That is, a skinny cord causes IUGR, rather than resulting from it.
Maybe it's time to look at cord substance and premature labor risk, too. These concepts are at least worthy of investigation. Because we know so little about the molecular biology of what we have to cope with every day, the only way we can operate effectively is to hold to whatever theory best explains what we observe and change that as soon as valid new information surfaces.
And, we will only know about that from seeking it out directly or via continued postgraduate educational venues and portals. Getting back to the example, what I see is not just that things are normal, but that humble bit of cord implies to me that all will be well, at least with fetal growth, subsequently.
RSNA 2014
As usual, I'm going to look silently at a lot of pictures. But I'm also going to be doing some active interviewing of manufacturers in two topic areas. First will be new transducer designs and new ways of reconstructing images, vital growth areas sometimes obscured by buzzwords.
I'm also interested in a few brand-new tablet or phablet systems that seem to deliver good image quality in a pocket-sized, wireless device with an HD display. I see these devices as physician-deployed physical exam tools, probably in conjunction with other remote sensors in the same package. And, if any manufacturer decides to make a holstered version, then I can have the private fantasy of the ultrasound slinger saving the day.
There is so much that goes into the development of new equipment, but I suspect there is a whole lot more -- much of it nebulous and hard to pin down -- that goes into using that equipment properly. There is more that goes into putting together all of the information we get, machine outputs included, to arrive at a conclusion that will be most helpful to each patient whom we are privileged to see.
Enjoy the meeting in every way you can.
Dr. Jason Birnholz was one of the few advanced academic fellows of the James Picker Foundation, and he has been a professor of radiology and obstetrics. He is a fellow of the American College of Radiology and the Royal College of Radiology, and he was an associate fellow of the American College of Obstetricians and Gynecologists.
The comments and observations expressed herein do not necessarily reflect the opinions of AuntMinnie.com.



















