
AuntMinnie.com presents the 24th in a series of columns on the practice of ultrasound from Dr. Jason Birnholz, one of the pioneers of the modality.
I love my ultraportable ultrasound unit; it empowers me. Now that I've been using it clinically, I may have a card printed that says, "Have Ultrasound, Will Travel."
I introduced the U-Lite (from the French company Sonoscanner) in my last column. This time, I want to tell you about my real-world clinical experiences. Before I used this device, I had thought that the "wrinkle" of portability would be where the system was used, but with full system performance, I believe the practice implications are a lot more extensive.
 Dr. Jason Birnholz.
Dr. Jason Birnholz.U-Lite's major advance is in overall image quality for all four of the currently available broadband-array transducers: a midfrequency phased-array sector scanner, a midfrequency convex array, and high-frequency linear and tightly curved endocavitary probes. Noise reduction is a part of image quality that I alluded to in the last column, but that is only part of the story.
Without prying into anything that might be a trade secret, I asked the developers why performance was so good. They said a lot of it has to do with the unique ways they have implemented transmit and receive focusing. I was awestruck; I had been so intent on image content that I had not realized the unit had a single, full-depth focal zone with no need to balance field-of-view, focal zones, and frame rate.
They said that the U-Lite determines time delays for echoes with nanosecond range precision. As a result, depth gates can be as small as a few tenths of a millimeter in body tissues, independent of transducer frequency. As for the mysteries of the software, I did a literature search and found that Dr. Bruno Richard, the company founder, published a theory of holographic focusing for ultrasound long before the U-Lite became a reality.
A lot of common uses of ultrasound are targeted or regional, i.e., directed at specific issues that do not require extensive knowledge about ultrasound. Medical expertise need not be too broad for those instances where the reason for the exam is specific and the range of findings is limited.
The following are some examples of this kind of usage for ultraportable ultrasound:
- Home-call nurses checking surgical sites on recently discharged patients
- Monitoring premature delivery risk in patients at home on bed rest
- Evaluating pain or fever after delivery
- Following chemotherapy responses for some tumors
- Onsite health screening at corporate campuses and health fairs, and via outreach programs for healthcare systems with community service priorities
 Figure 1: The 1946 M.D. Garage is a historic landmark in Cuyahoga Valley National Park in Peninsula, OH. All images courtesy of Dr. Jason Birnholz.
Figure 1: The 1946 M.D. Garage is a historic landmark in Cuyahoga Valley National Park in Peninsula, OH. All images courtesy of Dr. Jason Birnholz.If the M.D. garage were a clinic site, it could have diagnostic ultrasound tomorrow. When I saw this scene, I liked the tall sign proclaiming "Pure," and I decided that a grayscale rendering would be most appropriate.
Physician users
What is really interesting is that with a physician user, there are about a zillion daily uses for ultraportable ultrasound within hospitals. I interviewed and became friends with Dr. Nicolas Thiounn when I was in Paris recently. He is a professor of urology who has gotten a lot of attention for pioneering partial nephrectomy and superselective intraprostatic cancer treatment. He has been very happy with his U-Lite, which he started using to identify or exclude hydronephrosis in referred patients. Now, he uses the U-Lite as an integral part of his physical examination of office and hospitalized patients.
Obviously, Nicolas knows much more about the urinary tract than I or any other nonexpert could. However, I am a lot more familiar with the byways of medical imaging than he. After all, we have both put in years of study and work in our own medical domains (and both of us as professors of our disciplines). I would trust him to take care of any of my own urologic needs. I presume he would be happy to have me read images for him.
But, if we were at the same institution, I do not know if he would have thought to ask me what ultrasound equipment he should get, although he made a perfect choice and maybe interspecialty relations are more amiable in France than elsewhere. I have always been supportive of ultrasound in other specialties where an instant, albeit limited, exam is definitely in the best interest of the patient. Radiologists should all be supporting this kind of technological diffusion. However, I don't think I've met a lot of fellow radiologists who provide that kind of guidance freely and happily to our colleagues.
Everything ultrasound
I wanted to evaluate ultraportable ultrasound in a general, first-encounter situation. This is a little like going back to the beginning when ultrasound was new and its uses had to be discovered. Haven't most of you thought about what you would do over if you had the chance and knew more than you did the first time around?
The first place I thought of was a local primary care clinic for indigent, mostly Hispanic patients. The clinic provides an admirable service in taking all patients when they come in. It survives on a publicly supported shoestring without any profit motive. Staff members do not perform procedures or have a lot of in-house diagnostic resources; they refer complex or urgent problems to local facilities that have indigent care services.
I had thought of picking out a few index applications and training the staff to use the U-Lite in an automatic mode, after which I envisioned returning to my postretirement life of photographing old gas stations and reminiscing about ye olde golden age of ultrasound.
Rethinking the plan
German Field Marshal Helmuth von Moltke coined the aphorism that no battle plan survives contact with the enemy. Ditto for my clinic plan. There was a physician/owner who did not seem to be around much. Evaluations and treatment plans were made by nurse practitioners and assistants. No one seemed to have any visual skills or knowledge of when modern ultrasound might be used.
So, I decided to provide the service myself. I requested that the staff members ask me if ultrasound might be useful for specific patients when they were in the facility. The staff are all perfectly bilingual, while, alas, I am not, so the patient interactions tended to be an educational and communicative trifecta. There was very little free space and just a few private, tiny exam rooms, coincidentally perfect for an ultraportable, battery operated unit. And, I loved being back in the trenches, even though I haven't been out of them that long.
A new patient coming to a primary or general care facility might have anything. That's hard to prepare for. The evaluation process can be streamlined, but it really cannot be simplified. Not many people appreciate the burden and responsibility of a diagnostic first contact or, for that matter, the rewards of uncovering an actionable diagnosis.
There were two philosophical tenets drummed into me when I was a resident in diagnostic radiology at Massachusetts General Hospital in the early 1970s. Or maybe that should be two out of many things that stuck:
- That I was to be a diagnostician who relied on imaging tools primarily, but not exclusively
- That I always strive to get the most information out of any study that I did or interpreted; I have always assumed that this is standard in all radiology training programs
I approached each patient at the clinic in a global manner, tailoring the exam to a degree by the complaint and by my understanding of prevalent conditions that would be expected for each patient in the hope of early recognition and disability prevention. I nearly always use multiple transducers during any exam and various combinations of transducer center frequency, bandwidth, and harmonics. One-dimensional and color-flow Doppler are adjuncts.
The protocol is loose, mainly organized in the order that I tend to scan different parts of the body. I orient scan planes to the axis of the target organ and I document a lot. Most exams are completed in five to 10 minutes. I prefer reviewing and reporting all cases of a session at the end of the day, although I pass on impressions to the primary caregiver at the time of the exam.
A range of cases
One of the first cases I was asked to see was a 23-year-old man with painless swelling of the right half of the scrotum for the previous five years. The patient wanted to know if this might affect fertility (figure 2).
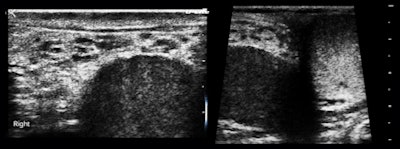 Figure 2: The right testis is embedded within a thick attenuating rind.
Figure 2: The right testis is embedded within a thick attenuating rind.Our impression was fibrous pseudotumor of the tunica vaginalis, which is a reasonably rare occurrence. There were no additional findings supportive of filariasis or schistosomiasis, which are even rarer with unilateral scrotal presentations. This case illustrates the challenge for the examiner to be familiar with the area he or she is imaging, or to know how to go from image findings to the proper reference source immediately.
This is a strength of radiology and one that we share uniquely with pathology. This particular example was easy, because the diagnosis is just a descriptive term, but we're not always as lucky. The clinic population has a high prevalence of cholelithiasis, obesity, hypertension, and metabolic syndrome (figure 3).
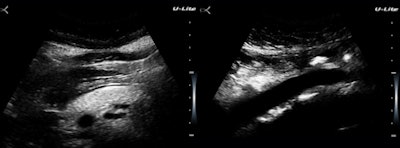 Figure 3: An obese woman with a fatty pancreas and a pristine aortic wall.
Figure 3: An obese woman with a fatty pancreas and a pristine aortic wall.There are two reasons why I am using up limited image real estate here with something as pedestrian seeming as a fatty pancreas. The diagnostic issue is not identifying obesity but in assessing cardiac and insulin resistance risks. Like fatty liver, pancreatic fat is a visceral fat deposition a big step closer to metabolic syndrome. The second is that the U-Lite does a much better job in the presence of obesity than I would have anticipated. Maybe this has to do with the submillimeter range gating?
 Figure 4: 7.8-week embryo.
Figure 4: 7.8-week embryo.The clinic does not see pregnant women, but there were a few unexpected but very joyous first-trimester surprises (figure 4).
Vaginal bleeding seemed to be a pretty common presenting complaint, and even the first few cases included examples of the range of causes separable by ultrasound: polyps (figure 5a), endometrial hyperplasia, and adenomyosis.
The polyp case was a woman with a three-year history and no diagnosis. The adenomyosis patient had heavier bleeding for almost the same length of time and was deathly pale when she presented during a clinic "ultrasound day"; anemia did not seem to have been a clinical consideration. The endometrium was reduced to a thin, denuded basal layer in another woman with a month of bloody flow (figure 5b).
I am including this case because it reminded me of a clinical pearl: Whenever you have vaginal bleeding without an ultrasonically visible cause, think of clotting disorders such as von Willebrand disease.
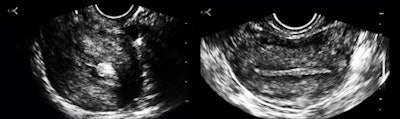 Figure 5a and b: A long-axis view of a retroverted uterus with stalked polyps and perhaps a touch of adenomyosis, and a transverse image of a normal fundal endometrium.
Figure 5a and b: A long-axis view of a retroverted uterus with stalked polyps and perhaps a touch of adenomyosis, and a transverse image of a normal fundal endometrium.'Incidental' findings
There were a number of "incidental" findings in this ambulatory, generally healthy population. Several women had benign-appearing thyroid nodules; one had a 9 x 16-mm mass with punctate reflectors, two small areas of capsule disruption, and a suspicious central vascular pattern, referred for biopsy. One asthmatic woman had pressure-sensitive, mediator-releasing subcutaneous nodules and a 38-year-old man had findings typical of familial multiple lipomatosis, albeit without an available family history, plus early, asymmetrical septal hypertrophy.
A 50-year-old man with mild cirrhosis had an abnormal prostate, and a 44-year-old man with unsuspected hypertension had a 17-mm left ventricle (LV) free wall thickness. One woman with a clinically undetected rock-hard mass in the upper outer quadrant of the right breast was found to have parenchymal hypertrophy and inspissated secretions in focal areas of duct ectasia. There were also musculoskeletal applications that I decided not to illustrate, as these were more like targeted applications in otherwise healthy people. I especially like "small parts" scanning at 16.6 MHz.
A 64-year-old man was being readied for transfer to an emergency room because the intake identified him as having chest pain. I noticed that he was sitting upright without any obvious distress, breathing slowly, and without diaphoresis or agitation. On inquiry, I was told that his heart rate was 72, his blood pressure was normal, and the automated analysis of the electrocardiogram was "normal." I asked to see him while the transfer was being arranged.
The patient was agreeable and very cooperative. He unbuttoned his shirt, and I did a quick cardiac survey: There was normal LV wall thickness; no asymmetrical septal hypertrophy; normal chamber proportions; great looking mitral, tricuspid, and aortic valves; and, most significantly, no regional LV wall movement abnormality. There was no pleural or pericardial effusion or dilatation of hepatic veins. He denied chest pain or dysphagia.
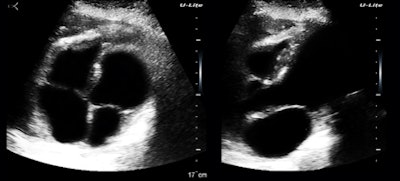 Figure 6: Apical four-chamber and mitral-valve views.
Figure 6: Apical four-chamber and mitral-valve views.I was thinking about the reflectors around the crux of the heart and how much of the apparent atrial volume disparity was a scan-plane effect when I continued looking and came upon something of more immediate concern (figure 7).
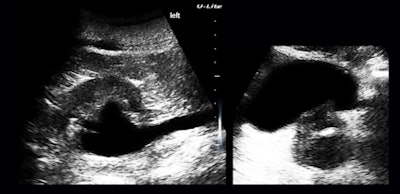 Figure 7: Hydronephrosis, hydroureter, and an abnormal prostate.
Figure 7: Hydronephrosis, hydroureter, and an abnormal prostate.I have the feeling that timely and expertly applied ultrasound, trusted fully by our referring colleagues, is a giant cost-saver by eliminating false alarms. We all focus on definite findings, whereas negative findings and normal appearances can be of enormous value in day-to-day practice.
I was entirely satisfied with equipment performance. I used the U-Lite exactly the way I would have used a max-performing high-end system, except both the patient and I were ambulatory and away from our usual haunts.
The clinic experience taught me a lot. The system we have inherited for ultrasound exams is referral for specified indications. I did not have the luxury of another physician prescreening patients at the clinic, so I did semiglobal exams and found something in almost everyone, which seemed to instill discomfort in the staff, who had no clear idea of how to utilize that information.
If you think about the usual referral process a little more, you will realize that "prescreening" is very insensitive, making the whole referral agenda inefficient. The nature of the "incidental" finding for ultrasound is unlike its cousins in all other imaging modalities. To crystallize this notion and get some sense of valuable ultraportable usage, I visited the polar practice opposite of the clinic, the neonatal intensive care unit (NICU).
A level III special care nursery
I was into transfontanelle scanning of preemie brains in the later 1970s. Studies done in the NICU have always been my clinical favorites, and their loss was my main regret when I moved to exclusive ambulatory outpatient work at the end of the 1980s. I liked the idea of an instant-starting, battery-operated, small unit for NICU use, and I visited one of the premier units in the Midwest.
I learned from my colleagues that the Children's Hospital of Philadelphia (CHOP) has been offering courses in neurosonography for neonatologists, and there is a groundswell of interest in neonatologists taking over this clinical application themselves. There was no ultrasound equipment available in the nursery I visited, however.
When they needed a study, a request was made to someone in radiology, who would dispatch a technologist, who would in turn lug a wheeled ultrasound unit there. Reports were provided electronically and quickly, but there were frequent disputes about interpretations based on images without direct clinical correlation. In addition, my colleagues expressed a need for identifying pneumothorax and for monitoring intravascular line and endotracheal tube placements, situations that need to be done instantly when the occasion arises.
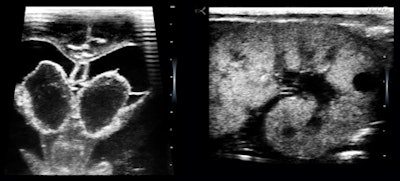 Figure 8: 27-week preemie with bilateral germinal matrix hematomas and polycystic kidneys.
Figure 8: 27-week preemie with bilateral germinal matrix hematomas and polycystic kidneys.The NICU is brimming with the most highly educated, proficient, and hardworking talent in the medical world. I have always felt that neonatologists should be scanning their own patients and that they should be able to look whenever they thought it might alter their management plans. When I used the U-Lite, I was interacting directly with neonatologists who intimately knew the babies I scanned, so we could go directly to the issues of immediate medical concern.
The lesson here is that just leaving an ultrasound unit in the NICU to be used by a technologist and interpreted elsewhere is not good enough. In this "conventional" mode, ultrasound tends to be used to confirm a clinical suspicion, not for identifying early signs or treatment surveillance.
Inasmuch as newborns can be anything from a 350-g preemie to a 5,500-g macrosomic infant, I thought their needs would best be served with a laptop unit on a small mobile cart, permanently and always stationed in the NICU, with a full complement of high-frequency transducers with different configurations.
Fantasies and conclusions
The basic thread of these experiences is the instant availability of a high-performance, low-noise portable device for both general and specific imaging tasks. High-performance, ultraportable ultrasound lets a physician leverage his or her specialized knowledge wherever it needs to be deployed, not as a replacement for more expert ultrasound or any other imaging procedure.
Radiologists are an already-trained user group with very broad clinical exposure. I see them as the primary users and beneficiaries of high-performance ultraportable equipment.
I spent the first half of my career wanting to become chief of a large academic radiology department and the second half avoiding that prospect. Avoidance was a lot easier than I like to admit. In my current fantasy role as a radiology strategist, I would equip every junior, senior, and chief resident, fellow, and staff member in my own department with a U-Lite to carry around.
I would want to be sure they were completely adept at ultrasound, and I would encourage them to use their personal devices on demand. Within the department, they could use ultrasound to supplement CT and MRI studies, biopsies, and other procedures, diminishing radiation exposure and facilitating throughput for those procedures. I would have them use their devices when evaluating patients before invasive procedures, and I would send them all around to take care of portable studies, which they would do in close cooperation with the primary care providers for those patients; ditto for outpatient clinics or remote facilities within the hospital network. These are the radiologists' equivalents of patient work rounds.
Obstetricians and cardiologists have decades-long experience and familiarity with ultrasound in their own specialty fields. I see them as instant adopters, taking the devices with them and using them during work rounds, in clinics or other locations where ultrasound is immediately available.
Did you wonder about "PDA" in the title of this article? That's my personal diagnostic assistant. Maybe I will start carrying mine in a quick-draw, echo-friendly holster.
Dr. Jason Birnholz was one of the few advanced academic fellows of the James Picker Foundation, and he has been a professor of radiology and obstetrics. He is a fellow of the American College of Radiology and the Royal College of Radiology, and he was an associate fellow of the American College of Obstetricians and Gynecologists.
The comments and observations expressed herein do not necessarily reflect the opinions of AuntMinnie.com.



















