AuntMinnie.com presents the 10th in a series of columns on the practice of ultrasound from Dr. Jason Birnholz, one of the pioneers of this modality.
Fellow Ultrasounder,
 Dr. Jason Birnholz.
Dr. Jason Birnholz.
I'm told that this column has become pretty well-read, for which I want to thank you and the editors of AuntMinnie.com. I really enjoy reliving the time when I was a professor and had the opportunity and great luck of lecturing all over the world. I always learned something from visiting ultrasound centers, more than the audience got from me. The most basic lesson was not to be doctrinaire about performing ultrasound.
There are a lot of equally valid ways to achieve our mutual goal of benefitting people through the use of this special imaging method, many of which may be much more clever and efficient than your familiar habits. Bad examples can help you avoid pitfalls too. Please use the message option on this page to let me know of topics you would like see in future articles. Remember to identify yourself, and say something about your facility and your role there.
I want to introduce a major everyday concern in ultrasound through two papers I wrote on separate fetal imaging tasks more than 30 years ago during ultrasound's wild frontier days.
Your child is a girl ... or a boy
When I submitted a paper in antenatal ultrasound assignment of gender for publication, a lot of my academic colleagues either harshly criticized the topic or just laughed at me. These were unpleasant, but not atypical, academic experiences. Interestingly enough, this paper was accepted and published in the New England Journal of Medicine (October 20, 1983, Vol. 309:16, pp. 942-944) without revision.
Obviously, using ultrasound to reveal fetal gender has thoroughly infiltrated the popular consciousness. I suspect that this one paper has generated a vast number of ultrasound exams over the intervening years, although I doubt anyone would ever confirm that.
In any event, gender determination is a simple anatomic imaging task, perfectly reliable, if you defer it until the genital tubercle has remodeled, 12 to 13 weeks, and reserve diagnosis until you have a clear view of the perineum with unequivocal delineation of external genitalia. This is especially important if you are using a noisy system and/or there is increased noise from adipose scatter, or if fetal depth or position obscure that portion of the body. There can be some difficulty between 12 and 16 weeks when tubercle remodeling is delayed slightly or there is physiologic clitoral prominence from an estrogen-enriched fetal environment.
I always look at fetal external genitalia, and that information is in every report. This is a holdover from my hospital days when I saw a lot of diabetic, hypertensive, and other "high-risk" cases in which there may be an elective early delivery to avoid fetal distress. Lung maturation and pulmonary response to steroids are earlier and better in females than males. If the patient wants to know, I show her on the screen. If she or her partner or spouse do not, then she will never even know that I have zipped past the area during my looking around.
From time to time, a patient will say to me something like, "I had an exam at ... and they wouldn't tell me if my child is a boy or a girl," or, what is much worse, "They wouldn't tell me anything." The issue here is withholding information, which is paternalistic, judgmental, and wrong, even given any of the obvious quibbles, such as the following:
- "It's really not that important."
- "It's not being withheld from the written report."
- "It's not in our routine fetal scanning protocol." (Is the spine, brain, or heart missing from the protocol too?)
- "Only the doctor can make that diagnosis (even though I make a lot of diagnostic decisions in deciding what images to take, and there is no doctor at this site monitoring me or any of the exams anyway)."
Trust
Trust is the basic factor in every aspect and type of medical care. Trust is binding and mutual between the patient and whatever facility or physician that patient selects. The nurse, technologist, or student who may be tasked with performing any kind of patient exam is the agent of the physician overseeing that procedure and inherits the same responsibilities, including conveying certainties for that procedure in a tactful and caring way.
Withholding information is a violation of trust. Trust is ephemeral and slippery; it has to be earned anew for each patient.
I perceived an issue of trust recently with the new maternal blood test for the most common fetal trisomies, frequently referred to as "cell-free DNA." Fetal DNA fragments get into maternal blood with trophoblast invasion of the myometrium, continuing as the placenta differentiates and expands.
The chromosomal parent of free DNA fragments is identified and counted. Autosomal chromosome fragment counts should be balanced; with a trisomy, the counts are unbalanced. Newer modifications utilize sequencing single-nucleotide polymorphisms (SNPs) for separation of maternal and fetal components of the sample. This test is highly sensitive and specific, about the same as chorionic villus sampling (CVS), which also samples the placental cell line.
The few companies offering the test have targeted trisomies 13, 18, and 21, and later added monosomy X. I use the test as often and as early in pregnancy as I can, in line with my preference for dual ultrasound and genetic wellness testing (i.e., www.amnionet.com) early in pregnancy.
I have used two companies providing this service. When lab 1 added monosomy X to its offerings, it made an arbitrary decision NOT to report fetal gender. This information is not that important to me, because I usually know what the fetal gender is, and the instances of phenotypic and genetic gender mismatches, such as adrenogenital syndrome, that might be detected are reasonably rare.
Nevertheless, I shifted to lab 2, which did not have that restrictive policy. If I know that some information is being withheld, then my trust in its reporting is undermined. This is actually a minimal form of the scandals over pharmaceutical companies suppressing reports of side effects. Lab 1 subsequently changed this policy, but my confidence in it had been tarnished, even though I respect and admire its technical accomplishments.
Perhaps, the relevance will be more apparent if you think of a patient as "I" and yourself as the lab. Even the calmest of patients is a little scared when having a diagnostic exam, and nothing exaggerates those anxieties like silence, especially to a pregnant woman, and particularly if she suspects that you are keeping something from her.
The eyes are the window to the soul
The second paper was about observing and characterizing fetal eye movements, done a few years earlier and reported in Science (August 7, 1981, Vol. 213:4508, pp. 679-681).
In the late 1970s and early 1980s, there was a lot of interest in pediatrics in extracting information from behavior. For newborns, there was particular attention to behavioral "states" and their transitions; term infants divide their time between deep sleep, active (or REM) sleep, and alertness, each with their own physiological steady states.
The most important diagnostic issue throughout the third trimester is what I think of as condition: Is the child healthy (leave alone) or about to get into trouble (deliver). Trouble means hypoxia, to which developing brains are particularly vulnerable. Growth retardation is a chronic, slow time-course problem with fetal compensations and a perceived increase risk of cerebral hypoxia.
However, the compromise may be rapid and overwhelming, such as sudden fetal death in diabetic pregnancy or with a cord accident. Condition is, as I see it, a concern in all exams when the fetus passes the point of potential viability, not just those few identified as "high-risk" or those for whom a biophysical profile is requested.
It is not enough to identify when a fetus may have already sustained a hypoxic injury to any organ. You really need to identify a risk of compromise, so that pre-emptive delivery may be accomplished before an injury is sustained. Since the brain is so exquisitely sensitive to hypoxia (and hypercarbia and acidosis), the idea is to have the fetus express some deterioration in its metabolic environment through a change in a brain-controlled motor activity, which is to say behavior.
You can look at the presence, absence, or pattern of respiratory activity; heart rate variability; or gross or fine motor behavior once you know the gestational norms for those factors. Fetuses at the outset of compromise do not enter active sleep states or do not sustain them. Heart rate variability, respiratory activity, and rapid eye movements are diminished or suppressed.
A sad case
There have been major improvements in our understanding of fetal and neonatal pathophysiology, as well as ultrasound performance and capabilities, since that paper from the late 1970s that provided one of the tools for this form of antenatal evaluation. Just a few years ago and definitely in our current era, I was asked to review images and reports for some ultrasound studies from a large university medical center.
Most of the records were withheld, and I am relying on memory. There had been a second-trimester ultrasound, reporting an anatomically normal fetus, and assigning gestational age. The next exam was maybe 31 or 32 weeks along. There were a lot of B-mode images that were all technically fine, and the report was short and limited to comments about normal growth. There was no use of Doppler. The images showed an obvious nuchal cord.
The umbilical cord is the conduit portion of the placental functional unit. Cords are pretty tough, and their structural integrity is increased by tight spiraling of the arteries around the vein. Cords with little or no spiraling are at higher risk for compression.
Nuchal cords are present in maybe as much as a quarter of all deliveries, and although there is hyperworry about cords during delivery (this is a main reason for all the heart rate monitoring during labor), nothing that happens that often normally is a really serious risk factor, all other things being equal.
Nuchal loops form and unform throughout the second trimester and are found in about 30% of all exams. In doing a routine exam, it is a snap to flip on the 2D Doppler to light up flow within the cord, identifying or excluding wrapping, as well as revealing the pattern of the cord insertion into the placenta. Nuchal cords can usually be compressed externally in multiparas, because the uterus is softer than in the first pregnancy. A normal physiologic response is an almost immediate increase in heart rate of about 20 beats per minute (bpm).
Back to the patient with the second-trimester ultrasound. There was another exam a few weeks later, apparently done because the patient was worried about a changed fetal movement pattern. The same facility -- in fact, the same examiner -- generated a series of transabdominal B-mode images, reported another set of measurements, and essentially nothing else. The images, however, very clearly showed that the nuchal cord had become very, very tight. The umbilical vein was fully compressed, and only the arteries were visible. There was a fetal demise a few days later.
I think that, in a legal sense, the negligence issue for that ultrasound facility has to be failure to report a significant finding, which is independent of the outcome of the case. I assume that all of the other guidelines, besides those of the American College of Radiology, specify fairly exactly the minimal applicable reporting guidelines for ultrasound exams.
There are obviously other issues in this case about the scope of the exam and the appearance (true facts unknown) of its being performed in an informational vacuum. The malpractice coffin nails were that the facility identified itself as expert and specialized in high-risk pregnancy, and that the reporting physician had co-authored a paper on ultrasound of nuchal cords in utero.
In the middle exam, the report might have said, "There is a single-loop nuchal cord that in our experience is unlike to be significant," if that is what they felt. Given that info, they might have at least glanced at the neck in the second exam, and having seen an impending catastrophe might have sought to exclude the occurrence of anoxic injury and expedited the patient's transfer for immediate attention.
Another nuchal cord case
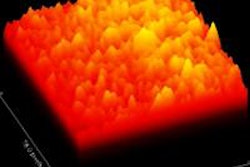
I recalled that case when I saw a primipara at 34.6 weeks, sent in because of suspected growth acceleration. A second-trimester exam had shown a normal-appearing male fetus and established the dating. The unexpected finding was a double-loop nuchal cord with some lengthy segments of diminished spiraling of the arteries. Multiple loops are generally thought to convey an increased chance of complications.
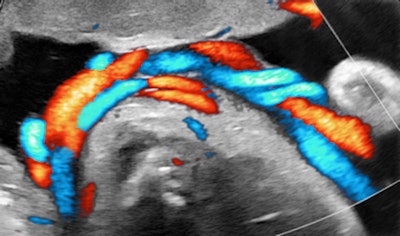
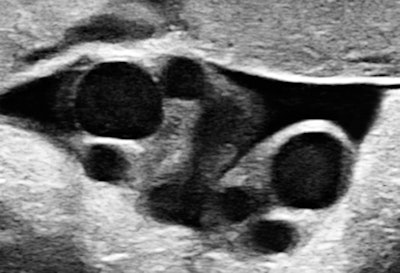 All images courtesy of Dr. Jason Birnholz.
All images courtesy of Dr. Jason Birnholz.
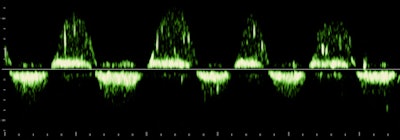 There are high-velocity spicules in the tracing. We have tended to think of these as microturbulence events, signaling the presence of surfactants in ejected lung fluid. This is unusual at the current gestational age in a male fetus, except when there has been repeated stress promoting lung maturation.
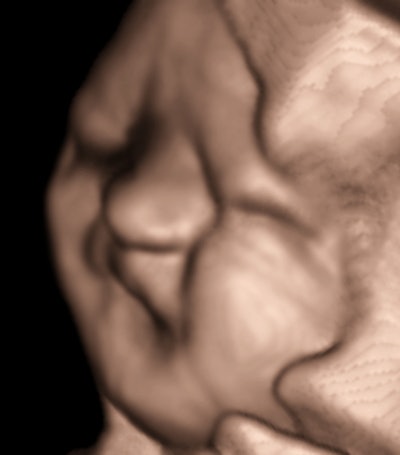
There are high-velocity spicules in the tracing. We have tended to think of these as microturbulence events, signaling the presence of surfactants in ejected lung fluid. This is unusual at the current gestational age in a male fetus, except when there has been repeated stress promoting lung maturation.We hit the panic button when we observed a lot of exaggerated head and torso movements (like aversive behavior) with a lot of mouth and tongue activity. I will leave it to you to decide what to make of fetal expression during one of the movement episodes.
Pulmonary maturation was confirmed, the patient was delivered, and the outcome was fine. Everything might have been equally fine with simple observation, but no one, including the prospective parent, thought the risk would have been warranted, even though the clues to problems were in the subjective, if not flaky, area of behavior.
But, isn't this just what a parent does when looking in on a child who is fussing or the practice of a nurse or pediatrician evaluating the need for attention of a newborn? We need to think of examining the fetus as our way of emulating a medical examination of a newborn. We cannot manipulate the fetus, but we have a giant advantage in being able to look within the body, as well as perusing just surface features.
Communication, communication, communication
What I have tried to do is to emphasize the importance of communication throughout the diagnostic ultrasound process, not just the one-way, timely sending of a written report. The communication vectors are between the patient, referring physician, examiner, and ultrasound physician. The report from the interpreting physician should include diagnostic doubts and uncertainties and also perceived technical limitations with the formal content. Reports, written notes, worksheets, and images are all part of the permanent documentation for each case.
The law does not and cannot require perfection. What is necessary is that we try to do our best and ensure that our effort and competence are on a par with other like facilities. The scientific content of the two early papers I cited is something that can be assessed, reconfirmed, amended, rejected, or updated pretty easily. At least it is subject to peer review. The way we apply those or other published findings in our examinations to an individual patient and how we communicate study content and conclusions are much more personal items that tend not to become public knowledge except in a very negative context.
I am sure that the sad-case facility typically does a great job. And, to be sure, late-pregnancy ultrasound exams stand on their own for ambulatory outpatient exams in terms of potential consequences of missed observations and misinterpretations. The procedural part of ultrasound may seem simple, but it can be, as you all know, exceptionally stressful. There are always worries: commiseration for the patients when there are problems, and our inner concerns -- "Have I done enough?" None of us is immune from lapses.
I wonder if lapses aren't something like drug side effects. You pick a drug for a patient and a condition with knowledge of how effective that agent is and what the side effects have been in a large population of people with prior use. That does not guarantee that it will be effective or that some adverse reaction will not occur. How might we decrease this kind of "side effect" and apply general guidelines to individual exams?
Trust, redux
Obviously, there is no magical answer, although a practical step might be to recast this in terms of trust. If I feel that I cannot establish a bond of trust with the patient, then I shouldn't do the exam, or if I cannot trust that I will see anything useful, then I ought not to do the exam either.
This might be a patient who is morbidly obese or someone who is referred for something that ultrasound cannot image. If a patient comes to our facility, I do not just send the person away. I almost always tell the patient that I doubt that I can help, but that I will look anyway for no charge. This has actually yielded some real surprises.
Being "trustworthy" seems to matter at least as much as technical competence. That may be too simplistic, but I believe that if you aim for this in every exam, you will be faultless.
Dr. Jason Birnholz is a graduate of Johns Hopkins School of Medicine and did his diagnostic radiology residency at Massachusetts General Hospital. He was awarded an advanced academic fellowship from the James Picker Foundation and has been a professor of radiology and obstetrics. He is a fellow of the American College of Radiology and the Royal College of Radiology.
The comments and observations expressed herein do not necessarily reflect the opinions ofAuntMinnie.com, nor should they be construed as an endorsement or admonishment of any particular vendor, analyst, industry consultant, or consulting group.