PET scans of people with psoriasis treated with anti-inflammatory biologics show the drugs may reduce vascular inflammation associated with cardiovascular disease, according to a study published February 8 in the Journal of Nuclear Cardiology.
A group led by Dr. Kevin Boczar of the University of Ottawa Heart Institute performed F-18 FDG-PET scans in psoriasis patients before and six months after treatment. The researchers found inflammation in the thoracic aorta of patients decreased significantly compared with healthy controls and suggest that biologics may also help mitigate vascular inflammation.
"These changes may be linked to changes in the coronary microvasculature in patients with psoriasis and support the notion that anti-inflammatory biologics may have a role in mitigating [cardiovascular] disease in this patient population," Boczar and colleagues wrote.
Psoriasis is an inflammatory skin and joint disease that is well known to be associated with vascular inflammation. Patients with the disease or its related arthritis (psoriatic arthritis) have higher than expected rates of cardiovascular disease and an increased risk of major adverse cardiovascular events. Biologics such as Enbrel, Humira, Cosentyx, and Stelara are a newer class of disease-modifying antirheumatic drugs developed to slow or stop the processes in the body that cause skin and joint damage.
Boczar and colleagues sought to explore any additional vascular effects of these four drugs, using F-18 FDG-PET scans to quantify inflammation in patients' thoracic aorta and comparing findings in individuals receiving non-systemic therapies and a healthy cohort.
The team conducted a study that included 34 participants, 11 of whom were psoriasis or psoriatic arthritis patients who were started on biologic agents; 13 of whom were psoriasis patients treated with nonbiologic therapies; and 10 of whom had noninflammatory arthritis and served as the control group. All patients underwent F-18 FDG-PET with low-dose CT at baseline and then another PET exam at six-month follow-up. To assess vascular inflammation, the researchers studied differences among patients in target-to-background ratios (TBR) based on FDG radiotracer uptake in the most diseased segment of the ascending aorta (TBRmax).
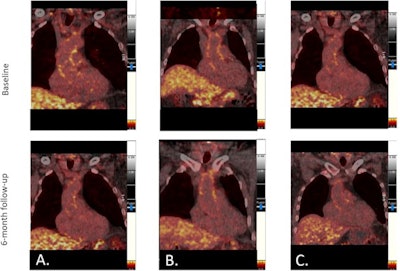 FDG-PET images showing change in ascending aorta FDG radiotracer uptake from baseline to six-month follow-up in (A) patients with psoriatic arthritis and/or psoriasis on biologic agents, (B) patients with psoriasis on nonbiologic agents, and (C) control patients with non-inflammatory arthritis. Image courtesy of the Journal of Nuclear Cardiology through CC BY 4.0.
FDG-PET images showing change in ascending aorta FDG radiotracer uptake from baseline to six-month follow-up in (A) patients with psoriatic arthritis and/or psoriasis on biologic agents, (B) patients with psoriasis on nonbiologic agents, and (C) control patients with non-inflammatory arthritis. Image courtesy of the Journal of Nuclear Cardiology through CC BY 4.0.The authors discovered a statistically significant reduction in vascular inflammation measured as FDG TBRmax in the ascending aorta in the biologic group only at six-month follow-up (baseline 2.84, follow-up 2.50, p = 0.033). They also reported statistically significant decreases measured as FDG TBRmax within the aortic arch (p = 0.002) and descending aorta (p = 0.007) within the biologic group but not the other groups.
"FDG uptake in the thoracic aorta decreased over the six-month study period compared to no change in psoriasis patients treated with non-systemic therapies or in a cohort of control patients with noninflammatory joint and skin disease," the researchers noted.
The results are consistent with a previous study of the effects of biologics in rheumatoid arthritis, which demonstrated a reduction in vascular inflammation on F-18 FDG-PET imaging after eight weeks of treatment, according to Boczar and colleagues. But the findings are not consistent with a placebo trial that showed no change in vascular inflammation on FDG-PET scans in patients randomized to Humira, phototherapy, or placebo for a period of 12 weeks.
These conflicting results underscore the need to interpret this study's findings with caution, the authors wrote.
"This study supports the notion that there is a positive impact of immune therapies on vascular inflammation and microvascular disease in patients with chronic inflammation ... but larger prospective clinical outcome trials investigating this are warranted," the group concluded.





















