CT shows that soft tissue changes after pancreatic ductal adenocarcinoma (PDAC) surgery suggest local recurrence, researchers have reported.
The changes include vessel encasement and luminal narrowing, wrote a team led by Tae-Hyung Kim, MD, of Memorial Sloan Kettering Cancer Center in New York City. Hyung's group found that on surveillance CT exams showing local recurrence after PDAC resection, new or increased soft tissue was present in 80% to 86%.
"[Our] findings … highlight features that most strongly indicate the presence of local recurrence or the likelihood of development of [it]," the team noted.
Pancreative cancer is the fourth leading cause of death in men and the third in women in the U.S., and PDAC makes up 90% of pancreatic cancer cases, Kim's team explained. PDAC recurrence rates after surgery stand at 80% within two years, but the best way to track potential recurrence has been unclear, with professional societies recommending different approaches.
To clarify the question, in 2023 the Society of Abdominal Radiology (SAR) PDAC Disease Focused Panel (DFP) published a consensus statement regarding postoperative imaging surveillance after PDAC resection, outlining which postoperative CT findings after PDAC surgery indicated possible local disease recurrence rather than postsurgical changes.
Kim and colleagues sought to evaluate inter-reader agreement and predictive effect of local recurrence imaging findings on surveillance CT exams after patients had undergone surgery for PDAC, using the SAR consensus statement as a guide. Their research included 126 patients who had surgery for PDAC between January 2009 and December 2014. Three radiologists reviewed baseline and postsurgery contrast-enhanced abdominal CT exams performed within two years, assessing features named in the SAR consensus statement such as surgical bed stranding and soft tissue, vessel encasement, main pancreatic duct dilatation, and ascites. The group calculated interreader agreement and the frequency of imaging features on follow-up CT imaging.
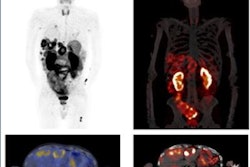
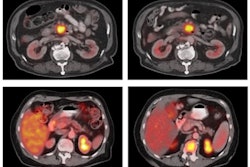
 57-year-old woman with pancreatic head adenocarcinoma who underwent Whipple procedure. (A) Axial and (B) coronal images in portal venous phase from baseline CT performed 3 months postoperatively. Based on three readers’ most common assessments, images show nodular soft tissue (arrow, A and B) at portocaval space near region of surgical clips, with associated encasement and focal luminal narrowing of superior mesenteric vein (dotted arrow, B). Clinical radiology report interpreted examination as showing postoperative findings. (C) Axial and (D) coronal images in portal venous phase from subsequent examination performed 6 months postoperatively. Based on three readers’ most common assessments, images show increase in size of nodular soft tissue (arrow, C) at portocaval space, with increased extent of narrowed segment in superior mesenteric vein (dotted arrow, D). Additionally, new luminal narrowing is observed at portomesenteric confluence (asterisk, D). CA 19-9 level was elevated at time of subsequent CT. Patient was diagnosed with locoregional recurrence. CT was labeled as recurrence CT. Image and caption courtesy of the AJR.
57-year-old woman with pancreatic head adenocarcinoma who underwent Whipple procedure. (A) Axial and (B) coronal images in portal venous phase from baseline CT performed 3 months postoperatively. Based on three readers’ most common assessments, images show nodular soft tissue (arrow, A and B) at portocaval space near region of surgical clips, with associated encasement and focal luminal narrowing of superior mesenteric vein (dotted arrow, B). Clinical radiology report interpreted examination as showing postoperative findings. (C) Axial and (D) coronal images in portal venous phase from subsequent examination performed 6 months postoperatively. Based on three readers’ most common assessments, images show increase in size of nodular soft tissue (arrow, C) at portocaval space, with increased extent of narrowed segment in superior mesenteric vein (dotted arrow, D). Additionally, new luminal narrowing is observed at portomesenteric confluence (asterisk, D). CA 19-9 level was elevated at time of subsequent CT. Patient was diagnosed with locoregional recurrence. CT was labeled as recurrence CT. Image and caption courtesy of the AJR.
Overall, 81 patients (64.2%) developed local recurrence developed two years after surgery. The team found that, on baseline postoperative CT imaging, independent predictors of eventual local recurrence were soft tissue for all three readers (odds ratio [OR], 2.78 to 6.85, with 1 as reference) and stranding for reader 1 (OR, 3.59), but that main pancreatic duct dilatation and ascites were not independent predictors of pancreatic ductal adenocarcinoma recurrence for any reader.
| Incidence of imaging features indicating local disease recurrence within 2 years after PDAC surgery on abdominal CT follow-up | |
|---|---|
| Feature | Percent incidence |
| New or increased stranding | 27% to 77% |
| New or increased soft tissue | 80% to 86% |
| Soft tissue with vessel encasement and luminal narrowing | 36% to 59% |
| New or increased main pancreatic duct dilation | 25% to 26% |
| New or increased ascites | 20% to 23% |
The study reveals the role of soft tissue in predicting local PDAC recurrence, particularly when associated with vessel encasement and luminal narrowing, according to the investigators.
"The findings overall support the recent SAR PDAC DFP consensus statement, while highlighting opportunities for continued optimization," they concluded.
The complete study can be found here.