New York City has been dramatically affected by the COVID-19 crisis, and neuroradiologists there were at times the first to identify the disease incidentally via imaging exams performed for other purposes, according to two presentations delivered on Monday at the virtual RSNA 2020 conference.
As the COVID-19 pandemic continues, radiologists must remain vigilant as they deal with everything from changes in workflow patterns to keeping families up to date on the status of their loved ones. Neuroradiologists from Lenox Hill Hospital, NYU Langone, and Weill Cornell Medicine shared their experiences in coping with COVID-19, and they offered best-practice tips for dealing with the crisis going forward.
Connecting with colleagues
In the spring, New York City was a COVID-19 epicenter, although the city was able to flatten the curve through rigorous lockdown efforts, said Dr. Christopher Filippi of Lenox Hill Hospital and the Donald and Barbara Zucker School of Medicine. Neuroradiologists were often the first to diagnose the disease as they encountered its manifestations on imaging ordered for other reasons.
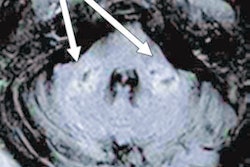
"Neuroimaging findings in the initial phase [of the pandemic] were incidental pickups when neuroradiologists were reading CT angiograms or spine cases," he said. "The second phase was dominated by strokes, hemorrhage, and large-vessel occlusions ... and in the third stage, encephalopathy dominated."
Filippi offered session attendees advice on how radiology departments can handle a COVID-19 surge, including the following:
- Stay connected with the various clinical teams.
- Act as a detective, looking for patterns that can inform diagnosis, treatment, and prognosis.
- Collaborate: Use local, national, and global networks.
- Be cautious about early literature. "We need larger, multi-institutional studies [on COVID-19]," Filippi said.
- Focus on teamwork. "It's crucial for patient care, education, and research," he said.
In the midst of a healthcare crisis like COVID-19, it's crucial to stay in close touch with colleagues, Filippi concluded.
"Dealing with a pandemic is stressful," he noted. "Reconnect and support one another."
Connecting with families
A pandemic demands not only close collaboration with clinical colleagues but also effective communication with patients and their families, according to Dr. Rajan Jain of NYU Langone Health. Jain described a program that the hospital put together called Family Connect in response to the need to keep COVID-19 patients' families apprised of a patient's status while also protecting clinicians' time.
The program included 65 radiology attendings and 150 attendings from dermatology, neurology, orthopedic surgery, pediatrics, and pathology, along with nurses and medical students. Nurses offered onsite support by helping families FaceTime with patients, as well as overnight support by responding to families' questions that came through the hospital's call center.
"Radiology took a leadership role in this program," Jain said.
Jain outlined the four key components of the program:
- Chart review to identify key patient information before rounds
- Interdisciplinary rounds via Webex or Zoom
- Calls to the patient's family contact
- Documenting the encounter in Epic
The average number of calls made to family contacts per day during the first wave of the pandemic was 276, and for the second wave it was 360. Of these, physicians made 46%, students made 42%, and nurses made 12%. NYU Langone surveyed its front-line healthcare workers and found that 85% felt the program helped them focus on direct patient care. In addition, 88% said it was critical for updating families about their loved one's clinical status, and 78% said that patient notes from the program helped them better care for patients.
"Through this program we were able to provide family members with timely and relevant clinical updates on a daily basis and support the Patient Experience team by responding to families' clinical questions," Jain said. "Family Connect allowed inpatient clinical teams to spend time on direct care and minimize time on the phone providing updates."
Neuroradiology's role
Beyond best practices for dealing with COVID-19 in the radiology department, there's no doubt that neuroradiology has an important role to play in the effective management of the disease, panelist Dr. Ajay Gupta of Weill Cornell Medicine concluded.
"COVID-19 isn't the flu -- it's much more serious in terms of extrapulmonary manifestations," he said. "And neuroimaging has often offered the first insight into COVID-19 positivity."