To help radiologists stay up to date on the ever-evolving coronavirus epidemic, an expert panel gave the lowdown on the current understanding of the coronavirus disease (COVID-19) and highlighted the points most pertinent to radiologists in an article published online on February 27 in Radiology.
As of February 26, the World Health Organization's tally of laboratory-confirmed COVID-19 cases has surpassed 80,000, including more than 2,700 deaths worldwide.
Most patients with lower respiratory tract infection from COVID-19 present with a combination of cough, fever, dyspnea, and myalgia, which progresses into acute respiratory distress syndrome (ARDS) in as much as 29% of the cases. The rate of death from COVID-19 is estimated to be roughly 2.3%.
With medical imaging playing a prominent role in detecting the disease as the outbreak continues to grow, it is becoming increasingly important for radiologists to remain knowledgeable on the topic, wrote the expert panel, led by Dr. Jeffrey Kanne from the University of Wisconsin School of Medicine and Public Health.
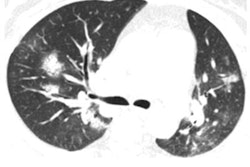
Thus far, findings on chest radiographs have been "difficult to interpret because of nonstandard and vague terminology," whereas CT has enabled radiologists to provide straightforward descriptions of COVID-19, they wrote.
"We advise all radiologists to be aware of typical chest CT findings of COVID-19," the panelists wrote.
After examining hundreds of submitted and published studies covering thousands of coronavirus cases, Kanne and fellow panelists found the predominant CT findings of COVID-19 to be bilateral, peripheral, and basal predominant ground-glass opacities, consolidation, or both. As much as 75% of patients have had CT scans showing peripheral focal or multifocal ground-glass opacities affecting both lungs upon initial examination -- features typical of an organizing pneumonia pattern of lung injury, and which have been peaking after about nine days, they noted.
From days nine to 13, the dominant CT findings have been crazy-paving pattern and consolidation. Following this period, and with appropriate management, the findings gradually begin clearing and have typically taken 26 or more days to resolve completely.
Recently, several studies have affirmed that the standard laboratory-based technique for diagnosing COVID-19, reverse transcription polymerase chain reaction (RT-PCR) testing, has a limited sensitivity of 60% to 70%.
These findings suggest that some high-risk individuals who have chest CT scans showing lung abnormalities may have COVID-19 despite initially negative RT-PCR results, the panelists noted. In addition, approximately 50% of COVID-19 patients may have normal CT scans in the first three days after onset of flu-like symptoms, emphasizing the value of extended surveillance.
"The importance of CT for detecting COVID-19 infection continues to increase as public health authorities grapple with the clinical complexities of early diagnosis," the panelists wrote. "Future challenges include distinguishing COVID-19 infection from other conditions that present with similar findings at radiography and CT."