
VIENNA - Spirometry and pulmonary CT parameters aren't helpful for predicting cardiac events in screening participants, even though such markers are independently associated with cardiovascular events in the lung cancer screening population as a whole, according to researchers from the Netherlands.
The group analyzed more than 3,000 participants from the Nederlands-Leuvens Longkanker Screenings Onderzoek (NELSON) lung cancer screening trial, testing the predictive power of spirometry, coronary calcium volume, emphysema, and bronchial wall thickness at CT. Only coronary calcium between screening years four and six was effective as a predictor of future events.
It's best not to waste time trying to use such measures for prognosis, the research team concluded.
"Coronary calcium volume does a much better job of stratifying patients into risk categories," so there's nothing to gain from using the other biomarkers to predict cardiovascular risk, at least in the lung cancer screening population, Dr. Richard Takx from University Medical Center Utrecht told AuntMinnieEurope.com.
On the other hand, it's perfectly feasible to assess coronary calcium using ungated lung cancer screening CT data, he said. While it's not as good as gated cardiac CT data, several studies show it works, and it's better than pulmonary markers for reclassifying patients into high or low risk categories for cardiovascular events.
This is all for the better because spirometry, for example, "is a pain in the neck" to perform -- much harder than calcium assessment, added Takx.
The association between pulmonary CT biomarkers and cardiovascular events is certainly logical, considering that chronic obstructive pulmonary disease (COPD) can be readily seen on CT, and studies have shown an association between COPD and cardiovascular events, he said.
"But these studies don't tell you if the reclassification is really better using these markers," Takx said. "Normally we stop at the hazard ratio. So it remains to be established whether these measurements contain relevant predictive value."
Prior studies "didn't really look at prediction for cardiac events, and that's what you want to do, you want to be able to say this patient has a higher or lower risk," he noted.
Therefore, for the current study, Takx and colleagues from two other Dutch centers aimed to assess the prognostic value of spirometry and quantitative pulmonary CT biomarkers for cardiovascular events.
The researchers analyzed data from 3,057 male lung cancer screening subjects in the NELSON trial who underwent spirometry and nongated chest CT on a 16-detector CT scanner at baseline, and at two, four, and six years thereafter. Age, smoking status, and number of pack-years were used as the base, and CT biomarkers were then added to these factors.
For the spirometry results, FEV1%predicted was calculated. FEV1% is the ratio of forced expiratory volume in one second (FEV1) to forced vital capacity (FVC). FEV1%predicted, in turn, is a patient's FEV1% divided by the average FEV1% in a certain population.
The researchers also calculated measures of pulmonary emphysema (15th percentile of the attenuation curve, or perc15) and bronchial wall thickness (10-mm lumenal perimeter, or pi10) based on the CT scans.
Finally, coronary artery calcium volume "was included as a kind of positive control" in terms of mortality risk and patient stratification, Takx said. The study's primary combined end point included fatal and nonfatal cardiovascular events.
The group performed a Cox proportional hazards analysis to determine the ability of spirometry and pulmonary CT measures to predict cardiovascular events. Kaplan-Meier curves were stratified by quartiles, and the study team calculated net reclassification improvement (NRI) and incremental C-indices as well.
The median follow-up time was 2.9 years (range, 2.7-3.3 years), and over that time 183 participants experienced a cardiovascular event, including both fatal (n = 16) and nonfatal events, Takx said.
Spirometry and pulmonary CT biomarkers were associated with an increased risk of cardiovascular events, he said. The adjusted hazard ratios for age, smoking status, and pack-years revealed little increase in the risk of events.
In contrast, the increased hazard for coronary calcium was significant. Coronary artery calcium volume had an adjusted hazard ratio of 1.046 (95% confidence interval [CI]: 1.034-1.058) per 100 mm3, a significant increase in C-index of 0.077, and a significant NRI of 17.3% (p < 0.0001).
"Coronary calcium volume showed a very clear trend [for increased risk,] especially in the first quartile and the third quartile, which were significant," Takx said.
| Spirometry and pulmonary CT biomarkers for cardiovascular events | ||||
| C-index | p-value | NRI | p-value | |
| Base model | 0.624 | |||
| Base + FEV1%predicted | 0.624 | 0.9236 | 0.6 | 0.7776 |
| Base + FEV1/FEC | 0.624 | 0.6199 | -0.1 | 0.9763 |
| Base + perc15 | 0.636 | 0.2200 | 3.7 | 0.2558 |
| Base + pi10 | 0.627 | 0.7279 | -2.2 | 0.4727 |
| Base + perc15 + pi10 | 0.638 | 0.1930 | -0.3 | 0.9414 |
| Base + coronary calcium volume | 0.701 | < 0.001 | 17.3 | 0.0001 |
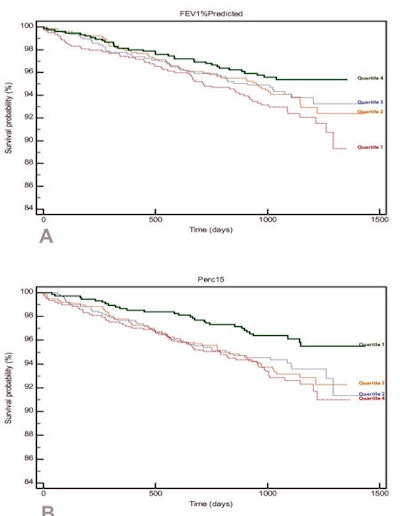 Kaplan-Meier survival curves for incident cardiovascular events per quartile. FEV1%predicted (top), perc15 (middle), and coronary calcium volume (bottom). Test for linear trend was performed across the quartiles and was statistically significant for all variables. Images courtesy of Dr. Richard Takx.
Kaplan-Meier survival curves for incident cardiovascular events per quartile. FEV1%predicted (top), perc15 (middle), and coronary calcium volume (bottom). Test for linear trend was performed across the quartiles and was statistically significant for all variables. Images courtesy of Dr. Richard Takx.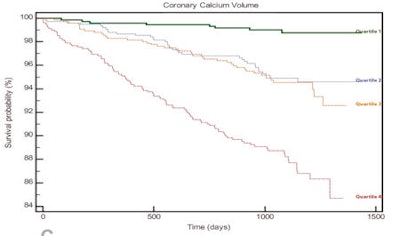
For predicting risk category, the results were mixed. None of the factors were significant in terms of pulmonary measures, while coronary calcium was highly predictive, with positive reclassifications in fully 17.3% of patients, Takx said.
"CT biomarkers and spirometry measurements, with the exception of FEV1/FEC, are significantly associated with cardiovascular events, but they do not contain clinically valuable independent prognostic information for cardiovascular events in male lung cancer screening patients," he concluded.



















