VIENNA - Which modality do you think comes with highest radiation exposure? That was the first question posed at yesterday's interactive teaching session E3 220 on acute abdominal inflammatory disorders. Delegates paused to watch the yellow countdown bar, as speaker Dr. Christian Hohl, head of radiology at Helios Klinikum, Siegburg, Germany, waited for an answer.
In this case, delegates were invited to look at a list that included ultrasound, radiography, small-bowel follow-through (SBFT)/enteroclysis, CT, and MRI. There were audible murmurings of 'CT' among the attendees, but when revealed, the answer produced some audible gasps of surprise: SBFT/enteroclysis, with 10 to 18 mSv for a typical abdominal examination, compared to CT's 7 mSv. However, depending on the CT procedure undertaken, Hohl admitted he would also accept CT as the joint top answer.
 Dr. Christian Hohl, head of radiology at Helios Klinikum, Siegburg, Germany. Image provided by ESR.
Dr. Christian Hohl, head of radiology at Helios Klinikum, Siegburg, Germany. Image provided by ESR.The session, part of the European Excellence in Education program, was a popular event, boasting a full audience. Delegates were treated to a succession of direct questions, while the seconds ticked away to reveal the top answers.
Learning objectives included knowing how to choose the appropriate imaging modality, becoming familiar with the patterns of distribution and appearance in imaging, and learning how to differentiate ischemia from inflammation.
"When a patient shows up with acute abdominal pain, what approach should you take?" Hohl asked delegates, pointing to the fact that patients presenting with acute pain were seriously ill, necessitating a host of steps from taking a medical history, physical examination, and laboratory testing. For imaging, choice of modality should largely depend on its sensitivity of detection for the suspected disease or condition, he said.
For most cases, requests for plain abdominal x-ray are inappropriate, pointed out Hohl, citing that in only 7% of cases does it influence clinical management, remaining negative or nonspecific in the rest. In comparison, MRI showed 100% sensitivity in the diagnosis of inflammatory bowel disease, abscess, and obstruction.
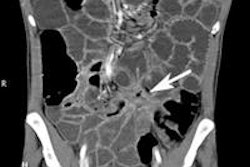
Delegates were also shown disease patterns ranging from appendicitis visualized on ultrasound and CT to the mural thickening, fat stranding, and comb sign of diverticulitis visualized by CT. Fat stranding and mural thickening along with visible lymph nodes in ultrasound were also signs of Crohn's disease; therefore, radiologists needed to know patterns of differential diagnoses on specific modalities for accurate and timely treatment.
Completing the session, Prof. Christoph Becker, professor of radiology at University Hospital of Geneva, Switzerland, outlined the advantages of techniques for imaging liver and bile ducts and described the typical findings in infrequent infections, in addition to providing specific tips on how to study obstructive jaundice.
Originally published in ECR Today March 2, 2012.
Copyright © 2012 European Society of Radiology