A study of more than 15,000 patients who underwent coronary CT angiography (CCTA) found that revascularization in patients identified by CT as high risk was associated with far fewer deaths than medical therapy (e.g., statins) alone. The results could be used to guide therapeutic decisions in patients with coronary artery disease.
Researchers from Cedars-Sinai Hospital in Los Angeles and several other international centers found that revascularization showed no apparent benefit in patients with lesser forms of coronary artery disease, according to intermediate-term follow-up (median, 2.1 years) of the patients.
"I think we've found an apparent anatomic threshold by CT where one might consider referral for invasive angiography," said lead investigator Dr. James Min in an interview with AuntMinnie.com.
The analysis, by Min and co-investigators Dr. Daniel Berman, Dr. Allison Dunning, Dr. Stephan Achenbach, and colleagues, was originally presented in poster form at the November American Heart Association 2011 meeting in Orlando, FL.
Question of mortality benefit
Prior observational studies of consecutive individuals undergoing invasive coronary angiography have shown a mortality benefit following revascularization in patients with very high-risk anatomic coronary artery disease, Min said. But to date, no studies have been conducted on any benefits associated with revascularization versus medical therapy in patients identified as high risk by CT.
Min and colleagues looked at 15,223 patients who presented with symptoms but without known coronary artery disease (CAD) who underwent CCTA at 12 sites in six countries. Patients were followed for a median 2.1 years (interquartile range: 1.4-3.3) for an end point of all-cause mortality. Obstructive CAD by CCTA was defined as 50% or greater luminal diameter stenosis in a major coronary artery.
The study examined stable patients with suspected coronary artery disease who were stratified after undergoing post-test coronary revascularization versus medical therapy, Min said. Researchers grouped patients into high-risk versus nonhigh-risk of CAD based on severity. Anatomic high risk included individuals with at least two-vessel coronary disease with proximal left anterior descending (LAD) involvement, three-vessel coronary disease, or left main artery disease.
The patients were part of the Coronary CT Angiography Evaluation for Clinical Outcomes (CONFIRM) registry that examined consecutive adults 18 years and older between 2005 and 2009 who underwent CCTA for suspected CAD. Individuals with known disease identified by prior myocardial infarction or coronary revascularization were excluded. Data on categorical risk factors and symptoms were collected prior to the scans.
CCTA scans were performed on a variety of scanner models (all 64 or more detector rows), with images analyzed on cardiac workstations. Investigators visually scored coronary segments for the presence of plaque using a 16-segment model, and patients were categorized by the number of vessels with 50% or greater intraluminal stenosis. Left main artery disease was categorized as the equivalent of three-vessel disease. The primary end point was all-cause mortality, and revascularization had to occur within 90 days of CCTA.
Cox proportional hazards model predicting death by any cause
|
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
According to the results, coronary revascularization in patients with high-risk CAD was associated with significantly lower rates of all-cause mortality compared to medical therapy alone. In contrast, there was no apparent benefit for revascularization in patients with other forms of coronary artery disease.
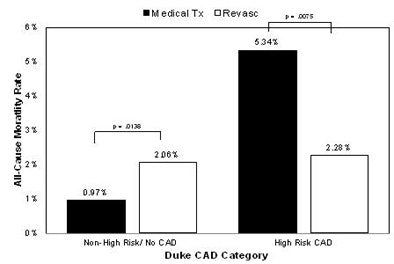 |
| Patients not at high risk for coronary artery disease (left two bars) had no statistically significant difference in their risk of death regardless of whether they were treated with revascularization or medical therapy. Patients at high anatomic risk of coronary artery disease (at least two-vessel coronary disease with proximal LAD involvement, three-vessel coronary disease, or left main artery disease) fared much better with revascularization than with medical therapy. Image courtesy of Dr. James Min. |
Mortality data broken down by one-, two-, or three-vessel disease are less robust than the high-risk/low-risk model because there were only about 1,100 patients who got revascularized. So for this study, "it's easier to just look at the binary high risk versus nonhigh risk," Min said.
In other study limitations, Min cautioned that the results are subject to the limitations of observational data. In particular, unobserved confounders and selection or referral biases may have affected the results. In addition, post-CCTA treatment was not mandatory; if it had been, it might have improved outcomes in high-risk patients.
The analysis may reveal an anatomic threshold of risk above or below which the patient might be better directed to revascularization or medical therapy, Min said.
"But in the nonhigh-risk group, there were still significant rates of mortality," he said. "I think we need to develop better tools to try to identify those patients who may have anatomically nonhigh-risk coronary disease, but who still need further evaluation for referral for invasive angiography and potential revascularization."
One potentially valuable tool that's coming of age is fractional flow reserve CT, which enables the identification of people who have nonhigh-risk coronary disease but significant amounts of ischemia caused by those lesions. Among lesions believed to be ischemic, about half show significant stenosis on CCTA and half do not, he said.