Juvenile obesity has ballooned in recent years, but imaging could play a role in deflating the problem.
At the 2003 Society for Pediatric Radiology meeting in San Francisco last month, Dr. Lane Donnelly from the Cincinnati Children's Hospital discussed a growing problem, and a method of distinguishing bad fat from worse fat.
In 2000 the U.S. Surgeon General's office estimated that nearly 15% of American children met the criteria for obesity, Donnelly said. Estimates for 2002 and 2003 are closer to 20%, and the figure is closer to 30% in the U.K. These children face a slew of risks, ranging from psychosocial trauma to coronary artery disease and diabetes.
"In addition to the risk factors, there is a problem with how the fat is distributed in your body," he said. "If you have a higher rate of intra-abdominal adipose tissue as compared to subcutaneous fat, then you have a much greater risk of developing coronary artery disease or Type II diabetes."
Assessing the ratio of these two types of fat was one goal of the group's study of 268 young women, all aged 22, who had been followed since age nine owing to their risk of obesity, Donnelly said. MRI has been used successfully in previous studies to assess this ratio.
"The only way to establish the ratio of intra-abdominal adipose tissue as compared to subcutaneous adipose tissue has been through cross-sectional imaging," Donnelly said. "Some have advocated getting a single slice with CT to get the radiation down, vs. doing the entire volume of the abdomen on the MRI."
Thus, the group sought to determine whether the data from a single abdominal slice can be representative of the entire abdomen. If the single-slice and volume protocols yield roughly equal measurements, then a single-slice exam in either MRI or even low-dose CT could easily be used to assess children's risk of obesity-related problems down the road, Donnelly said. And there is hope that troublesome obesity scores could spur parents and their children into making beneficial lifestyle changes.
In each subject, the group performed three MRI acquisitions of the entire abdomen, in 5-mm slice thicknesses from the T-12 level to the iliac crest. The acquisitions were as follows:
- The workhorse protocol was standard T1-weighted spin-echo. This technique makes fat stand out brightly for easy segmentation.
- The group also acquired T-1 weighted 3-D spoiled gradient-echo images. Data can be acquired in seconds compared to minutes for other protocols, making this method ideal for use in a screening setting.
- Last was the T1-weighted Fast Dixon protocol. This sequence can segment the MRI data into a water-only sequence, a fat-only sequence, or a combined sequence, Donnelly said. The fat-only sequence offers easy fat segmentation.
Data from the L3-4 disk space level was then assigned as the representative "single-slice" data. Regression analysis was used to measure intra-abdominal adipose tissue (IAT) and subcutaneous adipose tissue (SAT) in this slice, and compare it to data from the entire volume. The L3-4 level has been used in previous studies, Donnelly said.
The volume was segmented using an in-house software program that relies on k-means clustering to segment the data by intensity level. Next, the areas of each individual segment were added up to arrive at total volume. This can be accomplished by either calculating the intra-abdominal fat and subtracting subcutaneous fat from the total, or more quickly by subtracting the subcutaneous fat total from the intra-abdominal value, according to Donnelly.
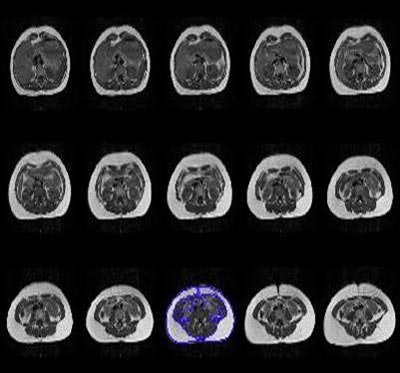 |
| Above, multiple abdominal MR images from a single subject demonstrate the entire volume of the abdomen. The color is on the image used to calculate the single slice data. Images courtesy of Dr. Lane Donnelly. |
"We used regression analysis to determine if the ratio calculated with the single slice of data accurately predicted (the result) when using the entire volume of data," he said. "Although it wasn't our primary goal -- and we have no gold standard for what the true ratio is because these are human subjects -- we also (analyzed) the variance (to determine) if the ratios determined by either the volume or single slice differ between the sequences."
The single slices were in fact representative of the total-volume results, Donnelly said. The mean IAT/SAT ratio calculated for each imaging sequence (single slice:ratio) was spin echo (0.16:0.20); Fast Dixon (0.15:0.19), and GRE (0.13:0.14). The Fast Dixon protocol provided the most accurate results.
There was a high correlation between the single-slice ratio and the volume ratio. And there was a highly highly statistically significant difference between the values obtained for the entire volume and the single slice among all three sequences, he said.
"Data from a single MR axial image can produce ratios representative of those calculated from the entire abdominal volume," Donnelly concluded. "And perhaps a single slice obtained from a CT scan may be a feasible option to MRI when evaluating obesity-related risks, particularly in adults, where radiation issues are not as great as in children."
An audience member said that if the technique is proven to be optimal, the exam could be a powerful tool for radiologists to intervene in the promotion of children's health.
By Eric Barnes
AuntMinnie.com staff writer
June 12, 2003
Related Reading
Gastric bypass battles bulge, but patients pose imaging challenge, March 27, 2003
Brains of obese may be wired to enjoy food more, June 27, 2002
Few gender differences in brain's response to food, June 7, 2002
PET scans show just seeing food lights up the brain, May 24, 2002
Copyright © 2003 AuntMinnie.com