From the patient's perspective, mandatory bowel prep may be virtual colonoscopy's biggest drawback. Sure, VC is less invasive, and it eliminates the small risk of perforation that can occur in conventional colonoscopy. But many doctors believe there will be no patient stampede to virtual colonoscopy until the prep gets easier.
As a result, researchers hoping to craft a kinder, gentler VC are looking at alternatives to purgation bowel cleansing. The possibilities include a partial prep combined with fecal tagging, as well as automated digital subtraction of fecal matter from CT image data, an imaging process akin to digital subtraction angiography.
At the April International Symposium of Virtual Colonoscopy in Boston, Dr. Phillipe LeFere from Stedelijk Clinic in Roeselare, Belgium, summarized his group's work using barium sulfate as a fecal tagging agent in virtual colonoscopy. Radiologist Dr. Michael Zalis from Harvard Medical School and Massachusetts General Hospital in Boston talked about digital subtraction bowel cleansing (DSBC), a process that combines barium and iodine fecal tagging with electronic bowel cleansing during image processing.
"If eventually (VC) could be performed without cathartic bowel cleansing, it would have (every) chance to become the method of choice in screening for colorectal cancer," LeFere said.
Along with colleagues Dr. Stefaan Gryspeerdt and Dr. Bartel Van Holsbeeck, LeFere conducted a multipart study to evaluate the use of barium sulfate as a tagging agent in prepless virtual colonoscopy. The first part, performed in combination with reduced cathartic cleansing, looked at the range of highest densities in fecal residue.
One hundred patients underwent virtual colonoscopy following two days on a low-residue diet (NutraPrep, E-Z-M, Westbury, NY), a dedicated 2.1% barium tagging agent (Tagitol, E-Z-M), and cleansing with magnesium citrate and 4 bisacodyl tablets on the morning of the exam. The images were reviewed to determine the effectiveness of stool tagging (density in Hounsfield units) and the amount of retained fluid.
According to the results, fecal residue was detected in 86/100 patients, mostly on the right side, including the cecum (66 segments), and the ascending colon (59 segments). Nontagged fecal residue was found in 7 patients. Densities ranged widely, from 20 to 2,890 HU, and much of the stool showed densities greater than 500 HU. The group concluded that the tagging was successful but not homogeneous.
"It could be that we didn't administer enough barium, or that we shouldn't administer it over two days," LeFere said. "The residual stool was mostly right-sided. This means that the right side of the colon (an important site for stool storage) will always be difficult to examine, and this could be a major challenge for electronic cleansing."
To determine whether different tagging protocols would produce corresponding differences in HU, the patients were divided into three groups, who underwent three different tagging protocols, combined with a strict hydration regimen of 1.5-2 liters of water a day.
"The first group had 3 doses of 350 ml of a 2.1% barium suspension. The second group started with a 4% suspension, followed by 2 doses of the 2.1% suspension. And finally, the third group was prepared for 3 days: the first day 3 doses of 50 mls of a 4% suspension, followed the next day by the same thing as Group 1. The best results (highest densities) were obtained in Group 3."
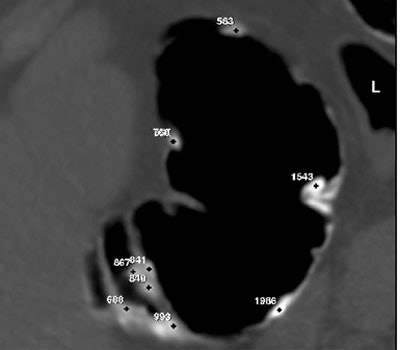 |
| Sample Hounsfield unit meaurements of barium-tagged fecal matter in patient groups 2 (above) and 3 (below). The highest HU intensities were obtained in the three-day regimen followed by patient group 3. Images courtesy of Dr. Philipe LeFere. |
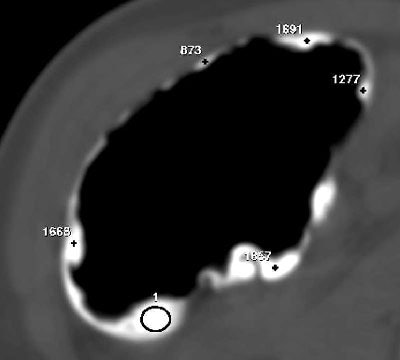 |
Both the water and fiber components of the stool were reduced significantly by combining the low-residue diet with a strict hydration regimen. "This resulted in both a reduction of stool volume and an increase in stool density," LeFere said. The study is continuing in an effort to optimize the tagging protocol.
Software cleans up after the fact
Anything that improves the patient experience will increase the number of patients who undergo screening, said MGH’s Zalis. His group is working to replace cathartic bowel cleansing with oral barium sulfate and iodine fecal tagging, followed by the application of digital subtraction technology.
"We're going to try to clean the image after the fact, rather than the patient," Zalis said.
"Following standard CT colonography, we employ specialized image processing software to remove the opacified ingested bowel contents, leaving the native soft-tissue elements untouched. The idea is to come up with an easier prep, and we're also going to attempt to preserve the 3-D problem-solving view, which a number of investigators have found particularly useful in terms of improving the confidence of evaluating CT colonography."
Efforts to perfect the technique have led to some engineering challenges. The researchers must design an algorithm that reliably subtracts contrasted fecal matter without subtracting soft-tissue lesions, Zalis said.
The subtraction process left a series of jagged edges that were visually distracting, so the researchers had to design a second algorithm to restore the native appearance of the mucosa. They are also looking into whether the radiologist is better served by reading the subtracted images alone, or by looking at both the native and subtracted images together.
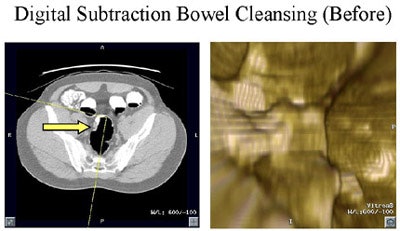 |
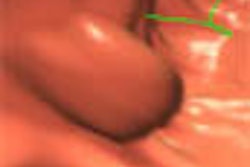
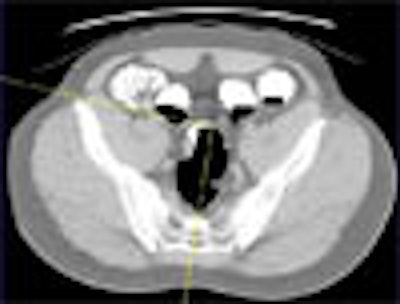
| Above: Forty-eight-year-old male with rectal bleeding. Axial (left) and volume-rendered endoluminal view (right) from CT colonography performed with digital subtraction bowel cleansing. |
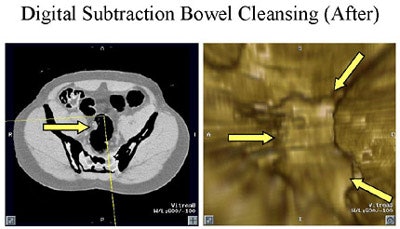 |
| Above: Following subtraction, the opacified, ingested bowel contents have been cleansed from the images by the postprocessing software, leaving colonoscopy-confirmed mass essentially untouched and visible on both axial and 3-D views. Images courtesy of Dr. Michael Zalis, Massachusetts General Hospital. |
In a study designed to measure and optimize the electronic cleansing process, Zalis and colleagues compared the imaging results in 55 patients in a screening population. They were divided into three groups using three different kinds of preps, and the resulting data were processed using the DCSB software.
Group 1 (25 patients) ingested nonionic oral iodine contrast (Oxilan) with meals for 48 hours prior to imaging with no other dietary modifications, with a second larger bolus just prior to imaging. Group 2 (25 patients) received diluted barium sulfate contrast (EZ-CAT) for 48 hours with a low-residue diet. Group 3 was a control group, and underwent standard cathartic bowel cleansing. "That additional bolus (in Group 1) helps in terms of opacifying the cecum," Zalis said.
The subjects performed self-insufflation with room air prior to undergoing low-dose virtual colonoscopy using 140 kVp, 50 mAs, 3.75-mm collimation and 1.8-mm reconstruction intervals.
In a subjective analysis, the DCSB groups (1 and 2) reported an overall decrease of 1.5/5 points in perceived discomfort compared to the control group. Patients preferred the iodine prep (Group 1) slightly over the barium (Group 2), Zalis said. Another test was designed to assess the homogeneity of the prep. This was accomplished by having the computer randomly select slices of interest in opacified segments of the colon, which were then read by two radiologists blinded to the results.
"The mean standard deviation for the colon segments using the barium is 170 HU vs. 123 HU for the iodine, and the difference between those two is also statistically significant," he said. "Iodine gave us a really good prep 72% of the time, whereas the barium did that only 32% of the time, and that difference was statistically significant. So from these data we came to a preliminary conclusion that iodine was the preferred method to opacify the colon for this type of prepless colonography."
Iodine appears to mix more thoroughly than barium with the ingested material, yielding a more uniform preparation, he said.
As for the bottom line -- polyp detection -- Zalis cautioned that he could provide only a very rough estimate based on a very small cohort of colonoscopy-proven cases using different preps. That said, sensitivity for lesions larger than 7 mm was 88% (7/8), and there was 1 false positive due to incomplete tagging. The technique detected 50% (3/6) of lesions 5-10 mm with no false positives, and 17% of lesions (1/6) from 1-5 mm. Average evaluation time was 11 minutes, versus 9.5 minutes for the traditional prep exam.
"We really need to evaluate this in a larger study, a project that is in process at our institution," he said. "Ultimately we want to test it in a really large cohort and get really good, stable estimates of its performance. We need to do a little more work in prep, and we'd like to couple this prepless system to a computer-aided detection system to see how the two perform together."
By Eric BarnesAuntMinnie.com staff writer
June 3, 2002
Copyright © 2002 AuntMinnie.com