Which patients are best suited for enterography? And if you have a patient who is a good candidate for the procedure, should you use CT or MR? Several enterography experts share their opinions.
On differing implications of active and fibrotic Crohn's disease
 Dr. Michael Gee, PhD, Massachusetts General Hospital
Dr. Michael Gee, PhD, Massachusetts General HospitalDr. Michael S. Gee, PhD
Associate Professor, Radiology
Massachusetts General Hospital, Boston
Active inflammatory disease and fibrosis have different indications with respect to treatment. Active inflammation implies on a histologic level that there are neutrophils -- a type of white blood cell -- and immune cells that are actively invading into the glands and crypts that are in the bowel wall, so that is fundamentally the basis for inflammatory bowel disease. It is almost an autoimmune type of inflammation in which the body's autoimmune system is attacking the bowel wall.
When we see active inflammation on imaging, this is an indication for medical therapies that are designed to block the body's immune response against itself. The most recent development has been these biological anti-immunomodulatory response agents for the treatment of inflammatory bowel, such as Remicade (infliximab) or a number of other agents in clinical trials. The premise of all those agents is that they blunt the immune response against the bowel wall. When we see inflammation, the implication is that this immune response is ongoing. It is an indication for the gastroenterologist to initiate or change that immunomodulatory medication regime to optimize immunosuppression.
In contrast, when we see fibrosis of the bowel wall -- mural fibrosis -- this implies that the immune response has died out. What you are left with is scarring in the bowel wall itself. When there is scarring, that typically causes fixed areas of narrowing that basically are refractory to medical treatment. So if you have a patient who has fibrosis, what typically happens is those areas of scarring cause bowel obstruction because they cause fixed areas of narrowing, and from time to time, patients develop these bowel obstructions because the food they're eating gets blocked by these strictures. So if a patient is symptomatic and has fibrosis, usually the only way to treat it is to surgically excise the area of stricture. That is the dichotomy between the detection of active inflammation and fibrosis and what it means to clinical outcomes and patient management.
On MR and CT enterography for pediatric patients
 Dr. David Bruining, Mayo Clinic
Dr. David Bruining, Mayo ClinicDr. David Bruining
Assistant Professor, Gastroenterology
Mayo Clinic, Rochester, MN
Many of our patients are diagnosed between the ages of 16 and 28, and many of them are considered for MR enterography. Particularly, the role of MRE is for patients who are quite young or have serial exams. I don't think the risk is huge as far as a single CTE exam is concerned, but what we try to do with each patient is to pick out the best exam for them. For patients younger than age 35 who have already had multiple CTs for other reason, I'll probably order MRE.
However, CT still has a role. In particular, the image acquisition time is much quicker for CT than MR. If I have a very sick patient, I'm worried about how long they will be able to tolerate being on a table. CTE is still my imaging modality of choice. If a patient is unable to follow commands, such as holding their breath, I may still ask for a CT.
This also applies to patients with tremors. For an obese patient or a patient I can't give glucagon to, I will probably perform CT.
Now with dose reduction techniques, I don't think the radiation will be as large of a concern. The short answer is that we look at these patients, and pick out the best modality for them and go from there. MR is particularly valuable for young patients who need serial exams.
On enterography for diagnostic small-bowel tumors and occult bleeding
 Dr. Khaled Elsayes, MD Anderson Cancer Center
Dr. Khaled Elsayes, MD Anderson Cancer CenterDr. Khaled Elsayes
Associate Professor, Radiology
MD Anderson Cancer Center, Houston
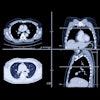
Among the various cancers that appear in the small bowel, enterography has the greatest value for diagnosing preoperative carcinoid tumors. By localizing carcinoid, you will be able to determine the segment of the bowel that should be resected. So preoperative planning is very important and also finding carcinoid.
These patients come to you when the tumor was not found anywhere else in the body. CT enterography is a very good tool to distend the bowel and to visualize and detect these small tumors. If there is any question about small-bowel carcinoma, CT enterography would be the modality of choice.
The other thing we quite often use CT enterography for at MD Anderson is detecting GI bleeding. This tends to be quite helpful for interventional radiologists to chase down the source of the bleeding to embolize it.
On the merits of enteroclysis for small-bowel imaging
 Dr. Dean Maglinte, Indiana University School of Medicine
Dr. Dean Maglinte, Indiana University School of MedicineDr. Dean Maglinte
Distinguished Professor, Radiology
Indiana University School of Medicine, Indianapolis
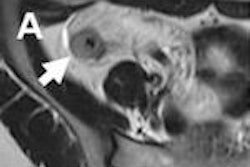
When you image the bowel, you need to distend it to be able to exclude any significant disease. To me, enteroclysis is the most reliable approach to rule out disease or confirm its presence.
It is especially valuable for detecting obstructions, for example. You have a patient with intermittent abdominal pain and nausea. You give them oral contrast, and you might not see the obstruction. But if you distend the bowel, the fixed area from some adhesions is easier to see. An adhesion will be exaggerated.
But if you are going to use enterclyosis, you must make sure you use conscious sedation. Nasal intubation is not comfortable. Patients will hate you for doing that, if you don't sedate them.
For transmural disease, the sensitivities for CT and MR enterography have been high: in the 80% to 90% range. But specificity is not as good for either CT or MR enterography, compared with CT or MR enteroclysis.
You won't see the scratches in the mucosa associated with very early changes associated with Crohn's disease with CT or MR enterography. But you can see them with a barium modification of enteroclysis, called air double-contrast enteroclysis, that has been very popular in Japan. With that technique, you can see the inner lining of the small intestine. It will allow you see those mucosal scratches.