Turkey is now leading the way in several areas of radiology and playing an increasingly important role in the European Society of Radiology (ESR), following a series of health system reforms and government-led drives to improve imaging in particular. In today's host session, "Turkey welcomes ECR," key figures from the country's community of radiologists provided delegates with a snapshot of their work, notably functional brain MRI, percutaneous treatment of liver hydatid cysts, and advanced hepatopancreaticobiliary imaging.
Building on their long experience in established diagnostic methods, Turkish radiologists have developed new interventional techniques that allow patients faster, more accurate diagnosis, and tailored treatment. In his introduction today, the president of the Turkish Society of Radiology (TSR), Dr. Abdulhakim CoŞkun, head of radiology at Erciyes University Hospital in Kayseri, discussed the challenges still facing this progressive modern republic and the impact on radiology, as well as the revolutionary health reforms that place imaging at the helm of patient care and ensure that more citizens than ever have access to quality services.
Turkish advances in interventional techniques took center stage among the scientific talks, specifically the role of the modified catheterization technique (MoCAT), a percutaneous treatment that can be used instead of surgery for complicated cases of cystic echinococcosis (CE), otherwise known as hydatid cysts.
Given the prevalence of CE at around 1% in rural Turkey, most imaging departments in the country encounter this condition on a daily basis. It is also endemic in Southern Europe, including the Balkan countries, southern Italy, France, Spain, and Portugal, and the incidence of the disease is increasing in Western Europe due to immigration and travel to and from endemic regions.
 Dr. Okan Akhan favors treating CE 2 and CE 3b hydatid cysts with a modified catheterization technique (MoCaT).
Dr. Okan Akhan favors treating CE 2 and CE 3b hydatid cysts with a modified catheterization technique (MoCaT)."Imaging and percutaneous interventional procedures for the treatment of CE is an important topic not only for the radiologists from the South and East of Europe, but also for Western and Northern European colleagues," said Dr. Okan Akhan, professor of radiology and chief of interventional radiology and abdominal imaging at Hacettepe University Hospital in Ankara. "Radiologists will come across this disease increasingly in their daily practice. However they will not always know what they are looking at. They may think that it is a simple cyst, but in reality the pathology is more complex and dangerous for the patient."
Diagnosis and classification of liver CE is based mainly on ultrasound, which is easy to use and allows visualization inside the cystic cavity to determine the contents and, thus, the subtype of cyst, he explained. After ultrasound, MRI and MR cholangiopancreatography (MRCP) are useful when communication between the cystic cavity and the biliary system is suspected. CT is less sensitive for demonstrating cyst content, but can be useful in defining the exact location of the cyst in the abdomen or liver if indicated, usually because the doctor suspects some kind of dissemination in the abdomen or thorax.
"Traditionally treatment was surgery, but this could lead to complications, and recurrence was high. In an era of interventional treatment, new techniques are now associated with lower major complications, lower mortality rates, and shorter hospital stays, as well as lower recurrence rates. Therefore, whenever possible, instead of surgery, the disease is treated by different percutaneous techniques, which in the long term are 98% successful," Akhan noted.
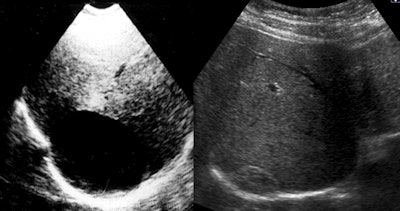 Ultrasound shows a liver CE 1 on the right side before the procedure in 1991 and a solid remnant with "pseudotumor appearance" -- 23 years after treatment. Images courtesy of Dr. Okan Akhan.
Ultrasound shows a liver CE 1 on the right side before the procedure in 1991 and a solid remnant with "pseudotumor appearance" -- 23 years after treatment. Images courtesy of Dr. Okan Akhan.Following on from their experimental study in sheep using a catheterization technique with hypertonic saline and alcohol, the Ankara group worked on a nonsurgical modified catheterization technique (MoCaT) based on complete evacuation of all cyst content, including the generated membrane and daughter vesicles, namely the fluid and the solid parts of the cyst. MoCaT, first described in 2007, has generated good results and low recurrence rates.
Radiologists should take a "stage-specific approach" to percutaneous treatment, Akhan believes.
"Although there are several classification systems for cyst subtypes, I prefer to use the WHO [World Health Organization] system as it reflects the natural history of the cysts better and gives us a chance to make differential diagnosis between the active and inactive subtypes," he said.
According to the WHO classification system, the major indications for percutaneous treatment of liver hydatid cysts include CE 1 (which should be treated by the puncture, aspiration, injection and reaspiration [PAIR] or catheterization technique), CE 2 (to be treated by catheterization or modified catheterization techniques such as MoCaT), CE 3a (treated by PAIR or catheterization technique), and CE 3b (treated by modified catheterization techniques).
Patients with CE 4 and CE 5 cysts should be followed up once a year by ultrasound using a "wait-and-watch" approach, because no treatment is indicated, Akhan continued. Surgery is the first-line treatment option for hydatid cysts that perforate in the biliary system, peritoneum, and pleura.
ECR delegates also learned about how to prevent dissemination of the disease into the abdominal cavity and sclerosing cholangitis. Complications such as recurrence, biliary fistula, and abscesses also were discussed, as well as their management.
"Turkey is leading the way in hydatid cyst diagnosis and treatment, even though it is a global disease. Turkey has a good imaging infrastructure, and radiologists are using their experience and knowledge base to gain pole position in this area with the development of new diagnostic and interventional techniques," said Akhan, who is involved in a European Union-funded research project looking into the incidence of hydatid cysts in Europe. "This is a widespread but neglected disease affecting mainly the poor, and, therefore, the drug companies are not paying that much attention to it. If someone becomes sick because of a parasite, we need to develop a simple medicine or vaccine to cure it."
Ultimately, this disease will vanish with improvements in living conditions that close the gap between the very rich and the very poor. Admitting that he won't be happy until the disease is eradicated from society, Akhan hopes to build on sophisticated techniques that result in lower mortality, while continuing to screen patients in rural areas and teach the MoCaT technique to other radiologists.
"I have published more than 20 papers on the topic and plan to continue. I want to change the available treatment options, particularly for CE 2 and CE 3b cyst sufferers," he concluded.
Originally published in ECR Today on 8 March 2015.
Copyright © 2015 European Society of Radiology