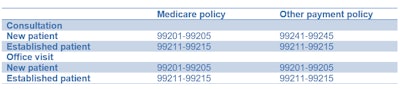
Proper coding of physician services is essential to efficient billing and the optimization of reimbursement from payors, including commercial and governmental entities. The current procedural terminology (CPT) codes issued by the American Medical Association (AMA) to describe physician procedures are supposed to be recognized as standards, but in practice they are not accepted equally by all payors. One example is CPT codes in the range 99241-99255 that describe consultation services. These are most often used by interventional radiologists.
 Sandy Coffta from Healthcare Administrative Partners.
Sandy Coffta from Healthcare Administrative Partners.In 2010, consultation codes ceased to be recognized by Medicare. Instead, Medicare requires the use of either a new patient office visit code for outpatients (99201-99205) or an initial day of hospital care for inpatients (99221-99223). Generally, payors other than Medicare have continued to accept the consultation codes, which carry a higher reimbursement due to the greater documentation and reporting requirements inherent in a consultation.
United Healthcare (UHC) recently announced that it would be phasing out payment for consultation codes 99241-99255 beginning in June 2019 under some of its provider contracts and by October 2019 for all providers. The immediate change will be for contracts that contain rates based on a Medicare fee schedule from 2010 or later, as those fee schedules do not include the consultation codes. UHC suggests that providers "modernize their fee schedules to bring them into alignment" with the Centers for Medicare and Medicaid Services' current relative value methodology before the October 1 date.
As a result of this change, the coding reference table in our 2017 article is not as clear-cut today as it once was. Rather than simply using the terms "Medicare" and "non-Medicare," we now must find out if a particular payor has adopted Medicare's policies or maintains the AMA's CPT coding definitions.
Evaluation and management (E&M) visits for the purpose of deciding whether to perform a procedure are generally billable and payable if they occur outside of the global period (GP). During this period, all services related to the procedure are included as a component part of the surgical package and, therefore, are not separately reimbursable.
However, for a procedure with a 90-day global period, considered to be a "major surgery," an E&M service performed on the same day or preceding day for the purpose of deciding whether to perform the procedure may be separately reported and payable with the addition of Modifier 57 (Decision for Surgery). UHC has indicated that they are not altering their global days policy at this time. See our interventional radiology coding article for more on the global period, including a table showing which procedures are subject to this rule.
This policy change by UHC might also modify the way documentation and reporting are handled. When a consultation code is used, the request for consultation must be documented, and the results of the consultation must be communicated by written report to the requesting physician according to the AMA guidelines. Presumably, UHC and others following the Medicare policy will no longer require these two elements.
UHC's action is not surprising. Commercial payors often adopt Medicare policies over time, particularly when doing so reduces their costs. The challenge for radiology practices and their revenue cycle management vendors is to keep on top of frequent shifts in payor policies.
Sandy Coffta is vice president of client services at Healthcare Administrative Partners.
The comments and observations expressed are those of the author and do not necessarily reflect the opinions of AuntMinnie.com.