Researchers from optical imaging technology firm NeuroVision Imaging and Cedars-Sinai Medical Center said their optical imaging system can identify retinal beta-amyloid protein deposits that mirror those in the brain, potentially enabling the early detection and monitoring of Alzheimer's disease.
The study, which was published online August 17 in JCI Insight, is the first to demonstrate the potential to image and quantify retinal findings related to beta-amyloid plaques noninvasively in living patients using a high-resolution retinal scan, according to senior author Maya Koronyo-Hamaoui, PhD, an associate professor of neurosurgery and biomedical sciences and a research scientist at the Cedars-Sinai Maxine Dunitz Neurosurgical Institute. Koronyo-Hamaoui, who is also a co-founder, inventor, and scientist at NeuroVision, said in a statement that the findings suggest optical imaging can serve as a surrogate biomarker for the investigation and monitoring of Alzheimer's disease.
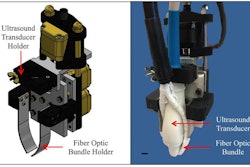
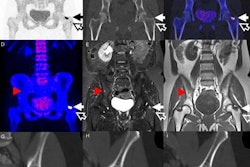
The Cedars-Sinai and NeuroVision approach consists of autofluorescence imaging of the retina using a specialized ophthalmic camera and image processing software. The JCI Insight paper included data from a 16-patient clinical trial, as well as new findings on Alzheimer's pathology in the retina from research on donated eyes and brains from 37 deceased patients -- 23 with confirmed Alzheimer's disease and 14 controls.
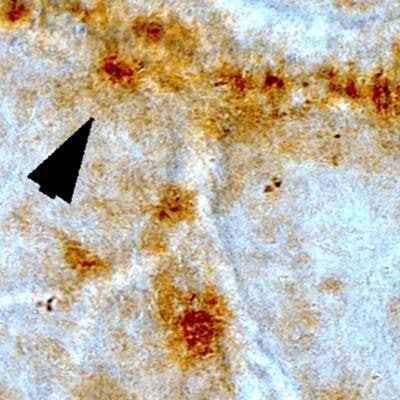
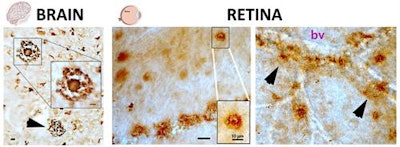 Images show the pathological hallmarks of Alzheimer's disease, beta-amyloid plaques (brown spots), as seen both in brain and retinal tissues from deceased patients. The structures of these plaques in the brain and retina are similar (classical and vascular-associated deposits; bv = blood vessel), suggesting that the retina faithfully represents the brain disease. Adapted from JCI Insight, Koronyo et al.
Images show the pathological hallmarks of Alzheimer's disease, beta-amyloid plaques (brown spots), as seen both in brain and retinal tissues from deceased patients. The structures of these plaques in the brain and retina are similar (classical and vascular-associated deposits; bv = blood vessel), suggesting that the retina faithfully represents the brain disease. Adapted from JCI Insight, Koronyo et al.The researchers found that Alzheimer's patients had a 4.7-fold increase in retinal plaque burden compared with controls. In addition, they said they performed the first histological quantitative analysis of retinal plaque clusters that contained the most toxic forms of beta amyloid with specific distribution patterns in previously unexplored superior peripheral regions.
The group also included the first report of certain Alzheimer's-related pathologies in the retina and demonstrated a significant correlation between retinal and brain plaques, with the coexistence of neuronal loss, according to NeuroVision. In addition, a fully automated calculation process for quantifying retinal autofluorescence showed a 2.1-fold increase in patients with Alzheimer's compared with controls.
In addition to participants from NeuroVision and Cedars-Sinai, the study team included researchers from the Doheny Eye Institute; Retina Vitreous Associates Medical Group; Retinal Consultants Medical Group; Sutter Neuroscience Institute; the University of California, Los Angeles; the Geriatric Research Education and Clinical Center; the Veterans Greater Los Angeles Healthcare System; and the University of Southern California.