Artificial intelligence (AI)-based analysis of body composition on routine abdominal CT exams can predict a patient's future risk of a heart attack or stroke, according to research published August 31 in the American Journal of Roentgenology.
In a retrospective analysis conducted on over 9,000 patients at Massachusetts General Hospital and Brigham and Women's Hospital, a research group led by first author Dr. Kirti Magudia, PhD, found that automated and normalized analysis of visceral fat area on abdominal CT revealed significant associations with subsequent myocardial infarction (MI) or stroke risk in both Black and White patients.
"Fully automated and normalized [body composition] analysis of abdominal CT has promise to augment traditional cardiovascular risk prediction models," wrote Magudia, now at Duke University School of Medicine, and colleagues.
Body composition analysis is increasingly demonstrating prognostic utility for a variety of applications:
- Monitoring patients with neuroendocrine tumors of a gastroenteropancreatic origin (GEP-NET) on PET/CT exams
- Predicting treatment outcomes in lung cancer patients
- Showing how the human body changes during aging
- Identifying elevated risk for ovarian cancer treatment complications
In the current study, Magudia and colleagues retrospectively analyzed 9,752 outpatients who underwent routine abdominal CT exams in 2012 and who did not have a major cardiovascular or oncologic diagnosis within three months of the scan. Of the 9,752 participants, 5,519 were women and 4,233 were men. The mean age was 53.2 years and 8,862 self-reported as white and 890 self-reported as Black.
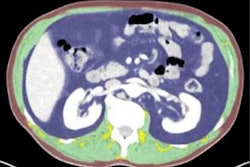
Next, the researchers utilized their previous deep-learning approach to perform fully automated analysis at the L3 vertebral level for three body composition areas: skeletal muscle area, visceral fat area, and subcutaneous fat area. Reference curves normalized by age, sex, and race were used to generate z scores for the three body composition areas. Any subsequent myocardial infarction or stroke among the participants was determined by a review of their electronic health records.
The researchers found that subsequent risk for MI and stroke for patients that the algorithm classified in the highest quartile of risk were higher than those classified as being in the lowest quartile, as measured by hazard ratio.
| Performance of AI for predicting MI and stroke risk by visceral fat area | |
| Hazard ratio of highest compared with lowest quartile | |
| Subsequent risk for MI | 1.31 [1.03-1.67] |
| Subsequent risk for stroke | 1.46 [1.07-2.00] |
The difference in hazard ratio for the highest quartile compared to the lowest quartile was statistically significant for overall effect (p = 0.04) for both MI and stroke when the AI algorithm analyzed visceral fat area. However, there was no association for subsequent risk of MI or stroke for normalized weight, body mass index (BMI), skeletal muscle area, or subcutaneous fat area.
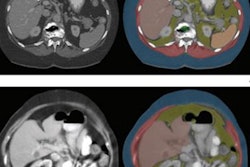
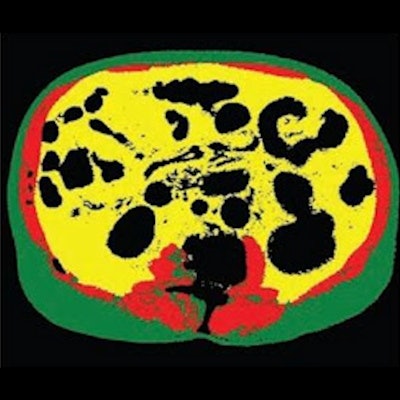
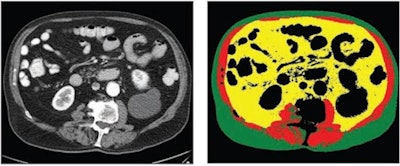 70-year-old white male patient with weight of 79.8 kg, body mass index (BMI) of 29.3, and low cardiovascular risk factors (nonsmoker, no diabetes diagnosis, blood pressure of 120/78). (Left) Axial CT image at level of L3 vertebral body. (Right) Matching automated segmentation label map. Visceral fat area z score is 1.41, corresponding to the 92nd percentile. Patient experienced both subsequent myocardial infarction and stroke. Images and caption courtesy of the American Journal of Roentgenology.
70-year-old white male patient with weight of 79.8 kg, body mass index (BMI) of 29.3, and low cardiovascular risk factors (nonsmoker, no diabetes diagnosis, blood pressure of 120/78). (Left) Axial CT image at level of L3 vertebral body. (Right) Matching automated segmentation label map. Visceral fat area z score is 1.41, corresponding to the 92nd percentile. Patient experienced both subsequent myocardial infarction and stroke. Images and caption courtesy of the American Journal of Roentgenology."[Visceral fat area] from fully automated and normalized analysis of abdominal CT examinations predicts subsequent MI or stroke in Black and White patients, independent of traditional weight metrics, and should be considered as an adjunct to BMI in risk models," the authors wrote.
Making use of reference values for age, sex, and race, the automated approach for body composition analysis could add prognostic utility to clinical practice by augmenting risk assessment beyond BMI and weight, according to the researchers.
"We anticipate that fully automated body composition analysis using machine learning could be widely adopted to harness latent value from routine imaging studies," they wrote.