The combination of 3D printing and augmented reality (AR) technologies can yield better outcomes for planning and guiding thoracoscopic surgeries than relying on virtual 3D lung models displayed on a monitor in the operating room, according to research published online December 1 in the Annals of Thoracic Surgery.
After comparing the methods in a study involving over 140 patients, a team of researchers led by Dr. Chengrun Li of the First Medical Center of PLA General Hospital in Beijing, China, found that surgeries utilizing 3D-printed lung models and AR were faster and had less intraoperative blood loss. These patients also had a shorter length of stay in the hospital.
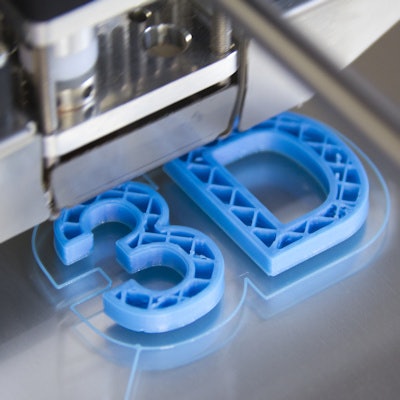
"The printed [3D] models enabled surgeons to see and touch interior structures of the lung," the authors wrote. "The augmented reality provided instant guidance to the surgery in the operating room. The combination of these technologies produced positive values in guiding laparoscopic lung surgery."
Although virtual 3D lung models have been used to guide thoracoscopic procedures such as segmentectomy and subsegmentectomy, these virtual models are not tangible for surgeons, according to the researchers. They hypothesized that if surgeons could physically manipulate a patient-specific printed model and then visualize it with an AR display during surgeries, this would enhance their anatomical visual and depth perception, and therefore improve outcomes in complex cases.
To test this hypothesis, the researchers studied 142 patients with early lung cancers who had been treated with thoracoscopic lobectomy, segmentectomy, or subsegmentectomy with wedge resection between June 2016 and October 2019. Of these patients, 87 had surgeries with virtual 3D lung models displayed on a monitor in the operating room, while 55 had procedures with access to 3D-printed models that were also displayed in AR during surgeries.
The 3D lung models were produced from enhanced CT thin-slice data using the MIMICS 17.0 software (Materialise Software) and an Objet500 3D printer (Stratasys). Four different colors were used to print the interior structures in the models.
In both patient groups, surgeons were required to discuss detailed surgical planning. Those in the group with 3D printing and AR performed their discussions by holding the 3D model. These surgeons then experienced surgery simulation using the Medical-Professional Augment Reality Display & Interaction Device (Co-Innovation Technology), according to the researchers.
While operating, surgeons used AR glasses and the printed model to track and identify segmented anatomy structures. However, those in the group without 3D printing and AR could only visualize the 3D lung model on the TV screen. The researchers performed propensity score analysis to minimize bias while comparing surgical outcomes between groups.
| Impact of virtual 3D lung models and AR on thoracic surgical outcomes | ||
| Virtual 3D lung model | 3D printing and AR | |
| Blood loss (interquartile range) | 33.75-60 | 22-46.25 |
| Operating time (interquartile range) | 78-107.25 minutes | 65-87.25 minutes |
| Length of hospital stay (interquartile range) | 4-5 days | 3-4 days |
| Evaluation scores by surgeons (interquartile range) | 89.75-92 | 96-98 |
The differences were statistically significant for blood loss (p = 0.006), operating time (p = 0.001), length of stay (p = 0.001), and surgeon evaluation scores (p = 0.001). The researchers found no significant differences between the methods in terms of complications and operating success rate.
"In the future, we are planning to investigate how these models can help our surgical residents to perceive lung anatomy and apply their mental perception into surgical practice," they wrote.