Faster and cheaper than surgery -- maybe even better than radiofrequency ablation -- a technique for percutaneously extracting lytic bone lesions in young adults has yielded impressive results at the Children's Hospital of Philadelphia.
"Osteoid osteoma is a small benign bone tumor, usually less than 1.5 cm in diameter," said Dr. Richard Towbin, chief of radiology at the hospital. "It affects children and young adults, usually in their second and third decades of life."
More than twice as many boys as girls are affected, some 2.6 to 1, Towbin said in a presentation at last week's Society for Pediatric Radiology meeting in San Francisco. The most common symptom is localized pain, usually more severe at night, and in 1/3 to 3/4 of the cases, aspirin and other nonsteroidal anti-inflammatories will relieve the discomfort, he said. The condition most often affects the long bones.
The trick is getting rid of it. In recent years, CT-guided percutaneous resection and radiofrequency ablation (RFA) have been gaining ground over surgery, owing to their comparative speed and lower cost. These days, Towbin and colleagues' interventional radiology team is in the enviable position of having their cases referred by orthopedists at their institution.
Since 1992 the team has performed the technique in 44 suspected osteoid osteomas in 40 patients, including 24 boys and 16 girls (mean age 11.4), all under general anesthesia. The patients had 25 lesions in the femur, 14 in the tibia, two in the knee, and a few lesions in the fibula, iliac, and scapula.
"Plain radiographs demonstrate the lesion as a sharply defined eccentric abnormality, usually round or oval, and there's reactive bone unless it's intra-articular," Towbin said. "The characteristic feature is a hyperdense nidus, which is the bullseye of the target in the lytic lesion."
Targeting usually begins with a plain radiograph. Then, for presurgical planning, the radiologists acquire 1-3 mm contiguous axial CT images in the region of the abnormality.
"We use CT for route planning and treatment planning, and we must identify the (best) route to avoid regional nerves and blood vessels," he said. "After local anesthesia is put into the skin, we insert the pins to target the lesion. Once we've proved the pin is in place with interval CT scans, then we'll drill the pin into the bone, and coaxially put a trephine over the pin and then cut the lesion out. Once the lesion is removed, then the tracks are cleaned and sterilized. As a learning process, we've realized that track length must equal at least 1.5 times the diameter of the lesion you're removing so that you can remove the back wall of the lesion intact."
K-wire can be used in place of Steinman pins, but the latter are bigger and stiffer and therefore easier to work with, Towbin said, adding that drills are easier to use than mallets.
Pathology samples were obtained in all cases, though not all were diagnostic, Towbin said. The procedure was technically successful in 100% of the cases, with 95% clinical success if one excludes the two patients who had recurrences at a mean 11.7-month follow-up, Towbin said. Negative outcomes were limited to two patients with postprocedural pain. Both patients with recurrences have successfully undergone the procedure again and are being followed up. The procedure time has been reduced to less than an hour per patient, and can be expected to drop even further as the process becomes more mechanized, Towbin said.
The patients are released after six hours of observation, usually with nonsteroidal anti-inflammatories and crutches to limit weight bearing.
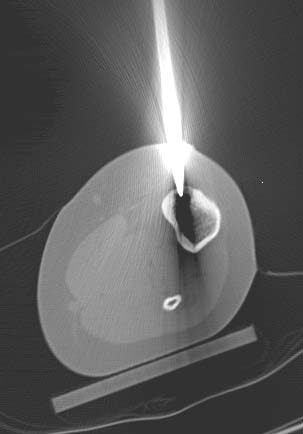 |
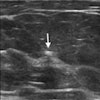
| Above, Steinman pin as it enters the bone. Image courtesy of Dr. Richard Towbin. |
Comparable to RFA
The same procedure using radiofrequency ablation has a comparable success rate. Radiologists treating a series of 47 patients at the Klinikum Rechts der Isar in Munich, Germany, were technically successful in 100% of patients and clinically successful in 44/47. Three recurrences were successfully treated (Journal of Vascular and Interventional Radiology, June 2001, Vol. 12:6, pp. 717-722).
And in a study at George Washington University Hospital in Washington, DC, 13 osteomas in nine patients were treated with RFA under general anesthesia after fluoroscopy-guided localization of the nidus. Two procedures initially failed due to failure to center the nidus using fluoroscopic imaging alone, but the technique was eventually successful in 8 of 9 patients, the authors wrote (Journal of Vascular and Interventional Radiology, March 2003, Vol. 14:3, pp. 375-380).
"We think that percutaneous removal of the osteoid osteoma results in a primary cure in most patients which is higher than ablation," Towbin said. "Both percutaneous methods are safe and effective, and we still will need further experience to see if one method is preferred over the other."
Asked to specify his reasons for preferring CT-guided resection, Towbin said that a few more steps are required to perform RFA, making it slightly more expensive.
"I think RF ablation has many positives," he said. "To some extent I think it's a solution looking for a problem, but I think the methodology ... has a lot of flexibility and uses, and as you know it's being used widely for a variety of lesions. I think the big question is what's going to be the primary cure rate, (as well as) costs and complications."
At the moment, the success rate for percutaneous resection is running a little higher than for RFA, he said, but this won't necessarily remain so over the long term. One advantage of resection is that a single procedure generally provides a cure, while RFA often requires multiple passes, sometimes on multiple occasions. Another advantage of resection is that histopathology produces better results in non-ablated tissue.
Ultimately, the comparative fracture rate may be the deciding factor between the two techniques, Towbin said.
"If resection, because it (creates) a larger bone defect, results in a high incidence or a significant incidence of fractures, I think that could become a pertinent negative," he said. "If it doesn't, then I think (resection) has the possibility of becoming the more dominant procedure."
By Eric BarnesAuntMinnie.com staff writer
May 16, 2003
Related Reading
Radiofrequency ablation shows promise in treating lung cancer, May 14, 2003
CT diagnoses peripheral T-cell lymphoma, with limitations, April 22, 2003
Percutaneous radiofrequency ablation may be an option for solid renal masses, April 21, 2003
Virtual endoscopy may have value in assessing auditory canal, October 11, 2002
Copyright © 2003 AuntMinnie.com