Virtual reality (VR) technology enables student radiographers in Australia to simulate the entire process of acquiring an accurate x-ray exam with greater efficiency and ease than with the standard training method of clinical role-play, according to a study published in the February issue of Radiography.
The group from Monash University developed a training program for medical professionals and trainees that allowed them to practice their conventional x-ray acquisition skills using a VR headset and controllers (Microsoft, Oculus Rift) in conjunction with hand-tracking software (Leap Motion). In early assessments of their VR clinic, lead author Daniel Sapkaroski and colleagues found that radiography students who used the VR simulation expressed greater levels of confidence in their capacity to position patients accurately compared with those who completed training with clinical role-play.
In the current study, the researchers expanded upon this prior work in order to explore additional potential benefits of simulating x-ray exams using their proprietary VR x-ray positioning simulation. The 75 student radiographers who participated in the study randomly received x-ray training with either the VR program or standard clinical role-play with real participants (Radiography, February 2020, Vol. 26:1, pp. 57-62).
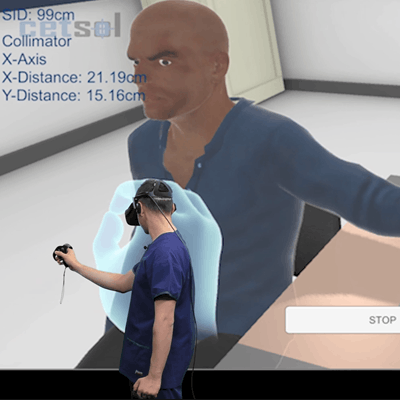
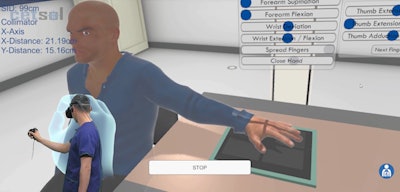 Virtual reality simulation for positioning patients undergoing hand radiography. Image courtesy of Daniel Sapkaroski.
Virtual reality simulation for positioning patients undergoing hand radiography. Image courtesy of Daniel Sapkaroski.Both training methods required the students to perform a series of steps, including the following:
- Selecting the correct imaging referral
- Identifying the patient in the waiting room and the correct type of exam
- Navigating the patient to the x-ray room
- Positioning the patient's hand for an x-ray exam
- Selecting appropriate parameters for the exam
- Discharging the patient
The researchers' qualitative evaluation of the students' performances revealed that there was no statistically significant difference in the students' positioning and radiography skills between the two training methods.
VR offered the added benefit of allowing students to work through the more challenging aspects of the process at their own pace and as many times as needed, whereas the clinical role-play group expressed a need for more practice time after the session had completed. What's more, the vast majority of students in the VR group (80%) said they would favor returning to the VR simulation over clinical role-play for future training.
"There was a strong similarity in common themes expressed by students ... a key point of difference identified was the benefit of repetition afforded by the VR simulation, in contrast to the need for more time using traditional role-play in a constrained laboratory setting," the authors wrote.
Since the publication of the current study, Sapkaroski and colleagues have expanded their VR clinical simulation program to include training for CT and radiation therapy for head and neck cancer. They have also developed a VR program that allows users to view and annotate DICOM files.
"There are some small differences in that the CT-centric VR program uses real DICOM data sets, compared to realistic 3D models used in the radiography module, allowing for a much greater level of dynamic positioning," Sapkaroski told AuntMinnie.com. "However, both rooms/modules are part of the one larger VR clinic and use the same communication engine."



















