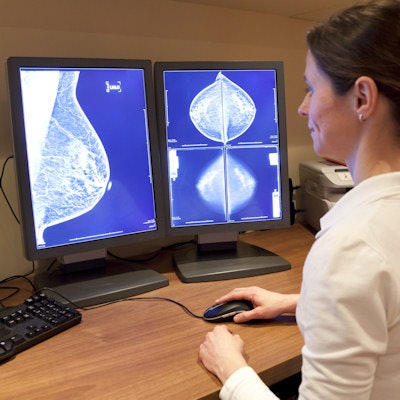
An artificial intelligence (AI) algorithm that analyzes mammograms and patient clinical information in electronic health records (EHR) can accurately diagnose breast cancer -- even in many cases in which cancers are missed by radiologists, according to research published online June 18 in Radiology.
A team of researchers led by Ayelet Akselrod-Ballin, PhD, and Michal Chorev, PhD, from IBM Research trained a combined machine-learning and deep-learning model that yielded an area under the curve (AUC) of 0.91 for predicting breast cancer. What's more, it identified cancer in nearly half of women who had an initial negative mammogram interpretation but were later found to have biopsy-proven cancer within a year.
Interestingly, the algorithm also determined that white blood cell profiles and thyroid function tests -- results that are not currently considered in published risk models -- were associated with breast cancer.
"The algorithm, which combined machine-learning and deep-learning approaches, can be applied to assess breast cancer at a level comparable to radiologists and has the potential to substantially reduce missed diagnoses of breast cancer," the authors wrote.
The researchers retrospectively gathered 52,936 images from 13,234 women who had received at least one mammogram between 2013 and 2017 at Assuta Medical Centers in Israel and had health records for at least one year prior to their mammography exam. The team then used mammography and EHR data from 9,611 women to train the deep-learning model to predict malignancy and to differentiate normal from abnormal screening exams.
For the purposes of the study, women were considered to have cancer if they had a diagnosis after biopsy within 12 months of the mammogram. After validation on 1,055 women, the algorithm was then tested on the images and clinical information of 2,548 women with a mean age of 55 years.
With 77.3% specificity at a model operation point of 87% specificity for predicting a biopsy positive for cancer, the model's results were well within the acceptable range of radiologists for screening mammography, as defined by the Breast Cancer Surveillance Consortium benchmark of 75% sensitivity and 88% to 95% specificity, according to the authors.
The researchers also emphasized that the model performed differently -- not better -- than the radiologists.
"In a scenario where double reading at screening mammography is not available, as is the case at Assuta Medical Centers, we believe that the use of this model as a second reader could be beneficial," the authors wrote.
The model doesn't use the same tools as radiologists for interpreting mammograms, for example, incorporating comparisons with prior mammograms or utilizing ultrasound images.
"We believe that, in the future, incorporating these data and additional clinical data such as genetic information can further improve the machine-learning/deep-learning model's performance," the authors wrote. "Machine-learning technology emphasizes the need for linking datasets from multiple modalities to improve the accuracy of breast cancer detection and save experts' valuable time on high-probability healthy individuals. In particular, this model's ability to lower false-negative results by half is of immediate clinical relevance."




















