If a picture is worth a 1,000 words, then the digital breast tomosynthesis (DBT) images are undeniably powerful: lesions that manage to hide on conventional mammography exams are easily exposed by DBT.
But does this dramatic improvement in tissue visualization lead to significant changes in the cancer screening setting? Yes, according to researchers at Boston's Massachusetts General Hospital (MGH). They noted a marked reduction in the callback rate for women screened with tomosynthesis at MGH.
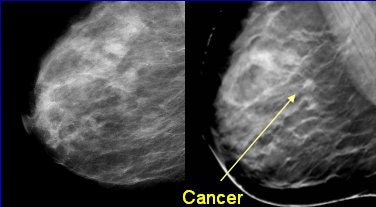 |
| Left, conventional full-field digital mammogram (FFDM). Right, DBT exam. All images courtesy of Dr. Daniel Kopans, senior radiologist at Massachusetts General Hospital, and Richard Moore, director of Kopans' breast imaging research projects. |
"We thought that we'd be able to measure callback reduction because a pilot study that we did back in 2002 suggested that the callback rate reduction might be as much as 25%," said MGH's Richard Moore during a presentation at the 2007 RSNA meeting in Chicago. "In 2004 and 2005, we were able to demonstrate a high-performance workstation (in order) to read tomosynthesis in the screening environment. In 2006, we did some studies to show the timing or how long it takes to read tomosynthesis (exams), which was an average of 35 seconds per case."
The current study is part of the National Cancer Institute's 3,000-women DBT screening trial that started in August 2005 using a clinical prototype DBT unit by GE Healthcare of Chalfont St. Giles, U.K. The detector on this second-generation DBT unit has an amorphous silicon sensor with a cesium iodide scintillator. Images are acquired in 15 projections with a 40° arc over 15 to 23 seconds with a rhodium anode x-ray tube for DBT. The gantry rotation is 360° and the unit, which permits all standard views, delivers the same dose as conventional craniocaudal (CC) and mediolateral (MLO) mammograms.
|
Having trouble viewing this clip? Click here to view full size clip or to change format. |
| Hamartoma with digital breast tomosynthesis. DBT has demonstrated the ability to reduce false-positive results. Courtesy of Richard Moore and Dr. Daniel Kopans, Massachusetts General Hospital, Boston. |
Moore and his co-authors, including Dr. Daniel Kopans, measured the callback rate for DBT compared with conventional four-view digital mammography (CM). They also categorized the callback rate by breast density, age, and compressed thickness. Moore and Kopans receive research support from GE Healthcare.
For this study, 2,233 screening DBT studies were performed on 2,114 women (ages 35-97) from June 2005 through the end of September 2007. Using standard clinical compression, one MLO view was acquired using DBT. Eight-iteration maximum-likelihood expectation-maximization (MLEM) reconstruction yielded one slice per millimeter of breast thickness. The DBT images were reviewed on a DBT workstation (DexTop Breast Imaging, Dexela, London) integrated into the PACS. They were read with previous study reference (DBT-P) and without previous study reference by two breast radiologists.
In that same time period, conventional mammography was done on 2,115 women (ages 35-97), yielding 2,233 mammograms. Standard mammograms with prior films (CM-P) and without priors were read by 10 staff radiologists with experience ranging from four years to 33 years.
 |
| DBT review workflow. Above, conventional mammographic prior images were automatically retrieved from PACS with CC and MLO views obtained as needed. Below, DBT MLO slice sets (35-85 slices spaced 1 mm apart) with 1800 x 2304 pixel in-plane presentation. |
 |
According to the results, the callback rate with DBT-P was 5.1%, 37% lower than the average conventional callback rate of 8% in a screening setting. The chart below details the DBT and CM reading outcomes paired with American College of Radiology (ACR) outcome scores.
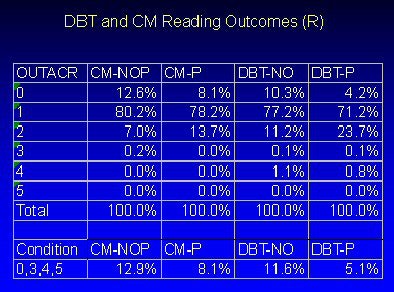 |
| Courtesy of Richard Moore. |
The authors also conducted a subanalysis, looking at the historical callback rate for Kopans (who read 91% of the studies). They found that with DBT-P, there was a 25.1% reduction in Kopans' historical callback rate (5.1% versus 6.8% with CM with priors).
Similarly, the group noted an improvement in callback rate with increasing experience for all readers. For example, during the first eight months, the callback rate for DBT-P was 6.3%, which dropped to 5.1% eight months later, and fell again to 4.5% after another eight months.
The majority of the women (60%) had ACR tissue density of 3. The mean compressed thickness was 54 mm. For those women with tissue type 3, the callback rate was 5.0% for DBT-P and 9.3% with CM-P.
Moore and colleagues acknowledged that the study did have its limitations, most notably that the callback rate results were generalized based on two readers, one of whom has 33 years of experience in reading breast mammograms. Substitute/coverage reading was done by co-author Dr. Elizabeth Rafferty, who has nine years of experience. In addition, these were single-view MLO studies, which may not visualize all the breast tissue, Moore said. However, the combination of CC and MLO views also suffers from similar limitations.
Nevertheless, "in the screening setting, we have a 25% lower callback rate compared to (conventional mammography)," Moore concluded. "Prior studies reduce the callback rate for DBT and conventional mammography."
RSNA session moderator Dr. Carl D'Orsi asked about the sensitivity of DBT. DBT appears comparable to CM in terms of its sensitivity, but the 3,000-woman trial is not powered to test for sensitivity, Moore explained. "Anecdotally, we don't miss cases with DBT," he stated. A one-year follow-up on subjects is under way to estimate the relative sensitivity of DBT in a screening setting, he added.
By Shalmali Pal
AuntMinnie.com staff writer
December 20, 2007
Related Reading
DBT: Not a panacea, but promising technology is unfairly panned, October 30, 2007
DBT unlikely to hit its target as savior of breast cancer screening, June 26, 2007
Copyright © 2007 AuntMinnie.com



















