Contrast-enhanced ultrasound (CEUS) lymphosonography is useful in identifying sentinel lymph nodes in breast cancer patients undergoing surgery, according to research presented November 29 at the RSNA annual meeting.
In her presentation, Dr. Priscilla Machado from Thomas Jefferson University in Philadelphia showed findings from her team's study of 81 patients, saying that lymphosonography is superior to radioactive tracers and blue dye in identifying these lymph nodes.
"All sentinel lymph nodes that were positive for malignancy were identified by lymphosonography," Machado said.
Sentinel lymph nodes are the first lymph nodes that drain from the tumor area in breast cancer. Because of this, the researchers said it is important to know if there are any metastases spreading from the breast tumor. Lymphatic drainage mapping is performed by either a blue dye injection or a radioactive tracer followed by surgical excision.
CEUS has been touted by researchers for using no radiation and providing real-time imaging as a vascular tracer. Previous studies have touted the success of lymphosonography, which uses the contrast agents found in CEUS to image sentinel lymph node presence in breast cancer patients.
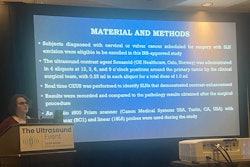
Machado et al wanted to look at the efficacy of CEUS lymphosonography in identifying lymph nodes for patients undergoing surgical removal of these nodes.
They looked at data from 81 women who underwent surgery for breast cancer to remove lymph nodes. The women received blue dye and radioactive tracer as part of their standard of care. The surgically removed lymph node specimens were scanned using color Doppler to confirm the uptake of Sonazoid, a contrast agent manufactured by GE Healthcare, and sent for pathology. The lymph nodes were classified as positive or negative for presence of blue dye, radioactive tracer, and Sonazoid.
A total of 241 sentinel lymph nodes were surgically removed from the women. Of these, 155 were positive for blue dye, 211 were positive for the radioactive tracer, and 212 were positive for Sonazoid.
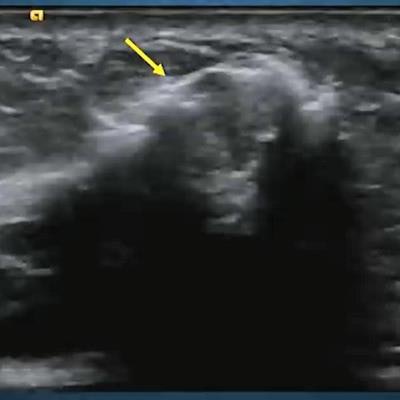
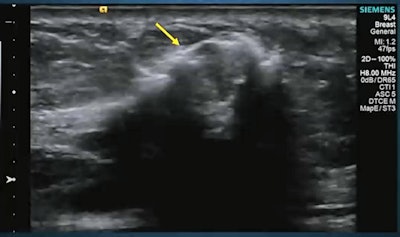 Sentinel lymph nodes can be identified through contrast-enhanced ultrasound lymphosonography (pictured), rivaling that of blue dye and radioactive tracers, according to research presented at the RSNA annual meeting. Image courtesy of Dr. Priscilla Machado.
Sentinel lymph nodes can be identified through contrast-enhanced ultrasound lymphosonography (pictured), rivaling that of blue dye and radioactive tracers, according to research presented at the RSNA annual meeting. Image courtesy of Dr. Priscilla Machado.Comparison with the blue dye reference standard showed that lymphosonography had 73% accuracy while the radioactive tracer's accuracy was 72%, although this did not achieve statistical significance.
When the comparison was done with the radioactive tracer as the reference standard, lymphosonography had an accuracy of 78%, while the blue dye injections were at 72%. However, this also did not achieve statistical significance.
Of the total lymph nodes removed, 34 were determined to be malignant by pathology. Of these, 18 were positive for blue dye, 23 were positive for radioactive tracer, and 34 were positive for Sonazoid. This translated to perfect accuracy for lymphonography (100%), while the accuracies for blue dye and radioactive tracer were 53% and 68%, respectively (p < 0.0001).
Machado said this is important in predicting the outcomes for breast cancer patients.
"The benefit is that you can do it before [surgery] and you can see the lymph node," Machado said. "A lot of times, what happens is, especially with the radioactive tracer, is that sometimes the lymph node you're interested in is below a group of lymph nodes and it takes all of them because your Geiger counter does not tell you which one it is."