Transesophageal echocardiography (TEE) is an "invaluable tool" for imaging critically ill patients with COVID-19, according to a May 23 Journal of the American Society of Echocardiography consensus statement written by more than a dozen cardiac imaging experts across the U.S. and Canada.
The statement was designed to provide guidance for physicians working in critical care environments during the novel coronavirus pandemic and is based on the authors' own first-hand experiences. The cardiac imaging specialists indicated specific situations when TEE may be better than transthoracic echocardiography (TTE) and other imaging methods for critically ill patients with COVID-19.
"While TTE remains the first-line modality for this assessment in the emergency and intensive care settings, TEE offers a reliable, safe, and powerful alternative for patients in whom TTE windows are inadequate or unavailable," wrote the authors, led by Dr. Felipe Teran, a clinical instructor from the division of emergency ultrasound at the University of Pennsylvania Perelman School of Medicine.
During the current pandemic, a TEE exam is most valuable when providing time-sensitive, goal-directed information for patients with COVID-19, the authors noted. It is also an important resource for visualizing the heart and lungs of critically ill patients who are not well-suited to other imaging methods.
One such use case is for patients with COVID-19 who experience cardiac arrest. The advantages of TEE for this population include shortened interruptions to chest compression and the ability to perform guided extracorporeal membrane oxygenation (ECMO) procedures, the authors noted.
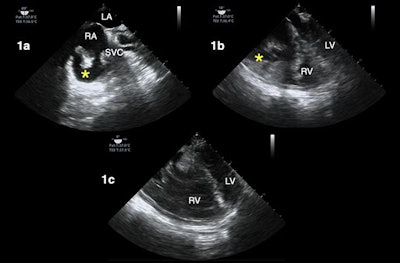 TEE during cardiac arrest resuscitation in a patient with COVID-19. The asterisks in image 1a and 1b highlight right atrial thrombus. Image 1c shows a dilated right ventricle (RV) and septal deviation during a pause in CPR. All images courtesy of the JASE.
TEE during cardiac arrest resuscitation in a patient with COVID-19. The asterisks in image 1a and 1b highlight right atrial thrombus. Image 1c shows a dilated right ventricle (RV) and septal deviation during a pause in CPR. All images courtesy of the JASE.TEE can also be used to image patients' lungs from within their esophagus, also known as transesophageal lung ultrasound (TELUS). This version of lung ultrasound may work particularly well for certain types of patients, such as obese individuals, those with surgical dressing, or those experiencing subcutaneous emphysema, the authors noted.
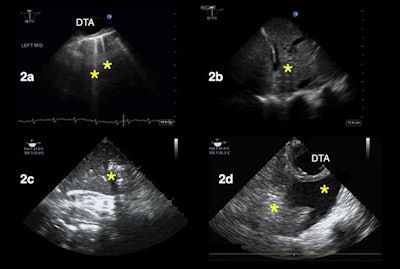 TELUS of patients with hypoxemia. In image 2a, the asterisks correspond to B-lines, suggesting increased extravascular lung water. In images 2b and 2c, the asterisks denote consolidation patterns, suggesting atelectasis instead of pneumonia. In image 2d, the left asterisk highlights an atelectatic lung, and the right asterisk points to a pleural effusion.
TELUS of patients with hypoxemia. In image 2a, the asterisks correspond to B-lines, suggesting increased extravascular lung water. In images 2b and 2c, the asterisks denote consolidation patterns, suggesting atelectasis instead of pneumonia. In image 2d, the left asterisk highlights an atelectatic lung, and the right asterisk points to a pleural effusion.Other use cases for TEE include evaluating the heart and lungs of patients who must stay in a prone position and those experiencing shock, a finding not uncommon in hospitalized patients with COVID-19, according to the authors.
"We have found that the TEE exam in prone patients has been particularly helpful during the COVID pandemic, given the degree of hypoxemia seen in these patients and the many urgent ECMO evaluations we've had to perform," the authors wrote.
While TEE may be helpful in specific situations, the decision to use TEE instead of another imaging method should be made on a patient-by-patients basis, the authors noted. They also advised implementing TEE at a hospital level, as the use of TEE requires the coordination of multiple departments and staff, including technicians.
"As resources are stretched in a pandemic scenario, the use of procedures and tools that promote efficiency and accuracy must be maximized," the authors concluded. "As such ... our group of experts from across North America strongly endorses TEE as an invaluable tool for managing the critically ill patient with COVID-19."