Ultrasound may be highly accurate for diagnosing pediatric appendicitis, but how does it perform for differentiating between perforated and nonperforated cases? Not very well, and that can pose a challenge when considering treatment options, according to research published in the March issue of Radiology.
In a prospective study involving nearly 600 patients with pediatric appendicitis, a research team led by Dr. Jennifer Carpenter of Texas Children's Hospital in Houston found that ultrasound offered more than 90% specificity but less than 50% sensitivity in diagnosing perforated appendicitis. A decision to pursue nonsurgical management for an uncomplicated case requires accurate differentiation between perforated and nonperforated appendicitis.
"On the basis of the results of our study, the risks and costs associated with CT must be weighed against the consequences of incorrectly differentiating perforated from nonperforated appendicitis," the authors wrote. "The results of [ultrasound] examinations with respect to appendiceal perforation cannot be interpreted in isolation and need to be considered in conjunction with the clinical history, physical examination results, and laboratory data."
On the bright side, the researchers discovered a number of ultrasound findings that had a statistically significant association with perforation.
Growing interest
Interest has grown recently in pursuing nonsurgical management of acute nonperforated appendicitis. While ultrasound is the preferred modality for diagnosing pediatric appendicitis, recent studies in the literature have shown the modality has high specificity but relatively low sensitivity for providing preoperative differentiation of perforated from nonperforated cases. Prospective studies with sufficient patient numbers to calculate reliable test performance measures have not yet been conducted, though, according to the authors.
As a result, Carpenter and colleagues set out to prospectively assess ultrasound's performance in differentiating perforated and nonperforated appendicitis in a large cohort of children. They also wanted to evaluate the association between specific imaging findings and perforation (Radiology, March 2017, Vol. 282:3, pp. 835-841).
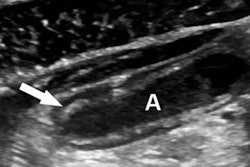
The researchers prospectively tracked all abdominal ultrasound studies that were performed at their institution for suspected pediatric appendicitis from July 1, 2013, to July 9, 2014. As per the center's protocol, grayscale and color Doppler imaging of the right lower quadrant was performed using a graded compression technique. The exams were interpreted for suspected pediatric appendicitis by one of 19 pediatric radiologists with a range of three to 40 years of postfellowship experience.
The ultrasound studies were interpreted using a structured reporting template and a risk-stratified scoring system:
- 1: Normal appendix
- 2: An incompletely visualized normal appendix
- 3: A nonvisualized appendix
- 4: Equivocal
- 5a: Nonperforated appendicitis
- 5b: Perforated appendicitis
The researchers then determined the diagnostic performance of studies that were designated as 5a and 5b. They also used multivariate analysis to correlate eight specific ultrasound findings with perforation: maximum appendiceal diameter, wall thickness, loss of mural stratification, hyperemia, periappendiceal fat inflammation, periappendiceal fluid, lumen contents, and appendicolith presence. For the purposes of the study, surgical diagnosis and clinical follow-up served as the reference standards.
Poor differentiation
Of the 577 patients who were diagnosed with appendicitis on ultrasound and met the study's inclusion criteria, 468 were diagnosed with nonperforated appendicitis and 109 were diagnosed with perforated appendicitis based on the scoring system. Surgical diagnosis showed, however, that there were 395 cases of nonperforated appendicitis and 182 cases of perforated appendicitis.
While ultrasound correctly identified appendicitis in 573 (99.3%) of the 577 patients, it did not perform well in differentiating between perforated and nonperforated appendicitis.
| Ultrasound performance in detecting perforated appendicitis | ||||
| Sensitivity | Specificity | Positive predictive value | Negative predictive value | |
| Ultrasound detection of perforated appendicitis | 80 of 182 cases (44%) | 364 of 391 cases (93.1%) | 80 of 107 cases (74.8%) | 364 of 466 cases (78.1%) |
"Even in a high-volume center with well-trained [ultrasound] technologists, the sensitivity for detecting perforation was low," the authors wrote.
Associations with perforation
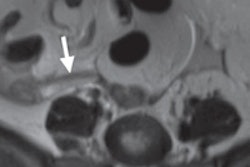
However, the researchers did discover that six findings had a statistically significant association with perforation.
| Findings associated with perforated appendicitis | ||
| Finding | Odds ratio | p-value |
| Longer duration of symptoms | 1.46 | < 0.001 |
| Increased maximum diameter | 1.29 | < 0.001 |
| Simple periappendiceal fluid | 2.08 | 0.002 |
| Complex periappendiceal fluid | 18.5 | < 0.001 |
| Fluid-filled lumen | 0.34 (a negative association) | 0.002 |
| Appendicolith | 1.67 | 0.02 |
"A longer duration of symptoms and several [ultrasound] findings are significantly associated with perforation, especially the presence of complex periappendiceal fluid, as well as greater maximum appendiceal diameter and the presence of an appendicolith," the authors concluded. "Particular attention should be paid to these imaging findings when interpreting [ultrasound] studies for pediatric appendicitis, especially when nonsurgical treatment is being considered."