An aging population of baby boomers will increase the need for cancer treatment facilities in Canada. But government health planners shouldn't rely on population and cancer incidence statistics alone to estimate radiation therapy resource requirements, according to an article in the February issue of Clinical Oncology.
A study of radiation therapy utilization trends in Manitoba from 2000 to 2009 revealed that medical staff workload at the province's sole radiation therapy treatment center consistently increased at a higher annual rate than the increase in the number of patients.
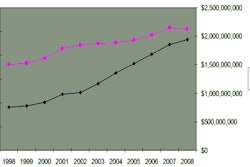
CancerCare Manitoba in Winnipeg experienced a 1.5% increase per year in the number of treated patients with incident cancer. However, the radiation oncology department averaged a 3.3% annual increase in the number of new patient consultations, from approximately 2,600 in 2000 to almost 3,500 by 2009. When researchers included follow-up treatments in their analysis, the actual increase per year was 3.9%, according to co-author Andrew Cooke, MD, a radiation oncologist.
The authors attributed the higher radiation therapy utilization to the availability of new technologies used to treat cancer, such as stereotactic radiosurgery and prostate brachytherapy. Workload increases were also attributed to time spent in the following:
- Longer consultations about treatment options with new patients
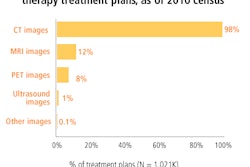
- Preparing one or more CT and/or PET/CT simulations
- Developing more complex treatment plans
- More detailed and extensive quality assurance reviews
Increasing use of hypofractionization regimes is reducing the overall number of treatments for some patients, the authors noted. As an example, the number of fractions per linac treatment course for breast cancer patients declined from 25 in 2000 to 21 by 2009. Overall, the number of fractions per linac patient declined by 2.6% annually.
The authors also pointed out that a shift to simultaneous integrated-boost treatment protocols may allow more patients to be treated with available equipment, improving overall staff efficiency. They acknowledged that increasingly sophisticated treatment planning software could also contribute to improvements in workflow.
Overall, the rapidly changing nature of radiation oncology due to technology innovation requires careful scrutiny by healthcare planners dealing with an aging population, the authors suggested. The Manitoba Bureau of Statistics estimates that the 65-years-and-older age group will increase by 21.7% between 2008 and 2018 and by 59.6% by 2028.
By Cynthia E. Keen
AuntMinnie.com staff writer
January 12, 2011
Related Reading
Radiation therapy volume grows as staff levels fall, October 28, 2010
Radiation oncology procedure volume edges up, report states, August 28, 2008
Copyright © 2011 AuntMinnie.com