Tracking patients with pancreatic ductal adenocarcinoma (PDAC) with annual endoscopic ultrasonography or MRI appears to improve clinical outcomes, researchers have found.
In fact, surveilling PDAC patients translates to an 84% one-year overall survival rate compared to a rate of 38% among PDAC patients who are not followed, reported a team led by Amanda Blackford of the Sol Goldman Pancreatic Cancer Research Center, Johns Hopkins Medical Institutions, in Baltimore, MD. The study results were published July 3 in JAMA Oncology.
"The findings of our cohort study show that high-risk individuals who underwent annual or semiannual surveillance [endoscopic ultrasonography] and MRI and who were diagnosed with PDAC had a greater likelihood of having smaller, lower-stage tumors; lower PDAC-specific mortality; and better overall survival … compared with a national cohort … matched for age, sex, race, and year of diagnosis and with similar tumor location and type of surgery … [and] the adjusted [hazard ratios] showed a fourfold higher chance of being alive for screened high-risk individuals," the group wrote.
PDAC is considered an incurable disease, and its incidence is on the rise, the researchers noted. Population-based screening is not recommended, but surveillance of individuals at high risk of PDAC could translate into earlier detection and thus increase overall survival time.
"While the overall survival for individuals with PDAC has improved in recent years, it remains poor, with approximately 11% alive five years after diagnosis," the investigators explained. "The majority of PDACs are diagnosed at an advanced, often locally unresectable or metastatic stage, which in turn directly affects survival."
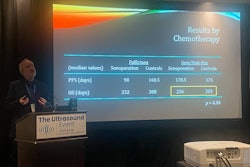
Blackford's group compared the survival rates of 26 patients with surveillance-detected PDAC (data came from medical centers participating in the Cancer of the Pancreas Screening program, which screens high-risk individuals with a family or genetic predisposition for PDAC) with 1,504 individuals with PDAC culled from the Surveillance, Epidemiology, and End Results (SEER) program. All patients underwent either annual endoscopic ultrasonography or MRI. The group tracked the stage of PDAC at diagnosis, overall survival (OS), and mortality from the disease.
The researchers reported the following:
- The median primary tumor diameter of the 26 high-risk, surveilled individuals was smaller than in the control patients, at 2.5 cm versus 3.6 cm (p < 0.001).
- High-risk patients were more likely to be diagnosed with lower-stage disease (stage I, 38.5% and stage II, 30.8%) compared with matched control patients (stage I, 10.3% and stage II, 25.1%).
- The PDAC mortality rate at five years from diagnosis was lower for high-risk tracked patients than the control patients (43% vs. 86%; p < 0.001).
- High-risk, surveilled individuals lived longer than matched control patients (median overall survival, 61.7 months vs. 8 months).
- The one-year overall survival rate was 84% among the high-risk, tracked cohort compared with 38% among the control group
- The five-year overall survival rate was 50% among the high-risk, tracked cohort compared with 9% among the control group.
The results indicate that surveillance of high-risk individuals diagnosed with PDAC could lead to the detection of smaller, lower-stage disease and thus improved survival, according to the team.
"[Our study suggests that] surveillance of high-risk individuals for PDAC using [endoscopic ultrasonography] and MRI within established programs at academic centers was observed to lead to the detection of smaller pancreatic cancers, a greater number of patients with stage I disease, lower mortality, and a much higher likelihood of long-term survival than unscreened patients in the general population diagnosed with PDAC," the group concluded.
The complete study can be found here.