One seemingly small mistake while performing an MRI study can result in a serious accident that might injure patients and staff or damage equipment. While the delegation of an MRI safety officer at each site is strongly recommended, few centers have as yet implemented this in practice. The situation looks set to change with the emergence of formal national and international guidelines that seek to minimize the risks for patients and professionals.
"MRI safety is just as important as radiation protection in other imaging modalities. Everyone has to appreciate the power of the magnetic field and the associated risks," said Csaba Vandulek, radiography services manager at Kaposvár University Health Centre in Hungary and also president of the European Federation of Radiographer Societies. "The fact that medical devices, such as respirators or patient monitors are classified as MR-compatible does not mean that they can be taken close to the MRI scanner. Manuals must be checked for every device."
Furthermore, not all medical devices or prostheses tested and classified as safe in 1.5 tesla are safe in 3 tesla or higher field strengths, he added. More tests are required to prove safety for such items, but limited resources and time restrictions often prevent these tests from being carried out.
 Operators must check the details of MRI-compatible equipment brought into the scanner room with extra care taken in the exclusion zone, Csaba Vandulek noted.
Operators must check the details of MRI-compatible equipment brought into the scanner room with extra care taken in the exclusion zone, Csaba Vandulek noted.Another common misconception stems from the idea that 3-tesla scanners now have better shielding than they used to, and safety issues are, therefore, of less concern than before, he pointed out. Conversely, professionals who spend the majority of their time working with high-field scanners may overlook the many risks and safety hazards associated with low-field systems when they suddenly swap shifts, erroneously becoming less cautious.
Vandulek illustrated this point with a personal anecdote from a large hospital outside of Hungary, where he was training staff on a 1.5-tesla scanner. On one occasion, the nurse who often administered the contrast agent approached a patient lying on a table near the scanner to prepare him for the injection. The nurse's scissors flew straight out of her pocket, only centimeters away from the patient's head and into the bore of the magnet.
"What I couldn't understand was how this could happen to a member of staff who had been working in the MRI department for some time. It was not her first time there. She was a regular," he explained, noting that the upshot is that staff can never be too careful, and nor should they underestimate MR.
To avoid complacency, Vandulek advocates regular compulsory MRI safety training and the delegation of an MRI safety officer at each MRI unit. This officer should be responsible for staff training, aware of the current safety rules and guidelines, and have the time and resources to keep up-to-date with MRI safety issues.
While the role of these officers is accepted and endorsed in the U.S., there are as yet no European requirements or official guidelines for a member of staff to fulfil this role at MR sites. The MRI Safety Working Group, which comprises key stakeholders from regional and international MR associations, is drawing up recommendations for maintaining MRI safety across the European Union. Part of this guidance pertains to safety officers, as many sites remain as yet without such an element in their MR staff team.
Vandulek believes that the safety officer should be actively involved in patient scanning and be well-versed in the 2013 updated guidelines from the American College of Radiology (ACR), the International Electrotechnical Commission (IEC) guidelines, and other national guidelines where they exist.
"It would be a mistake to specify one set of MRI safety guidelines for the whole MRI community. It is best for the officer to develop internal protocols based on international guidelines, but in line with local practice and adapted to the equipment used at the site," he noted. "I believe that in future, MRI radiographers will have a key role in ensuring a safe environment and practice at MR imaging facilities across Europe."
While officially termed a refresher course for radiographers, today's session targeted all professionals involved in MRI, not just those relatively new to the modality.
 Extensive knowledge of the applications and limitations of a scanner's pulse sequences will help operators avoid artifacts, according to Sofia Brandão.
Extensive knowledge of the applications and limitations of a scanner's pulse sequences will help operators avoid artifacts, according to Sofia Brandão.Sofia Brandão, radiographer in the MR Unit at São João Hospital in Porto, Portugal, covered the main characteristics of sequences for the most frequent studies in the clinical setting during her talk, which also underlined the basic principles of patient management in the clinical -- and research -- environment.
"Imaging patients in the clinical setting is quite challenging, in the sense that their cooperation and physical characteristics or clinical condition may force us to adapt or shorten the imaging protocol or the pulse sequences, while maintaining the focus on good diagnostic image quality," Brandão told ECR Today.
Her hospital has an MR unit with two systems (1.5 and 3 tesla) and a team of six radiographers who each have between six and 16 years of full-time scanning experience, and who each perform around 3,500 scans per year.
"The radiographers work solely with MRI and have full autonomy during scanning. We actively participate in pulse sequence optimization and suggest alternatives, both in clinical and research work. There is full coordination between radiologists, neuroradiologists, and the radiographers in both fields," she said.
The team of radiographers undertakes all kinds of examinations, from research functional MRI to clinical cardiac and dynamic pelvic floor imaging.
Brandão believes high-field MRI allows for increased benefits in spatial resolution or advanced applications, but there are more artifacts such as those associated with magnetic susceptibility or dielectric effects.
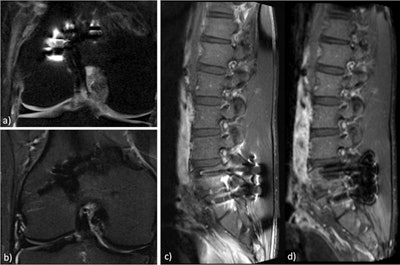 Fat suppression may be quite challenging whenever metallic materials are present. The fat-sat technique (a) may be replaced by short tau inversion recovery (STIR) (b) when the evaluation of the cartilage is not the main focus of the exam. In cases of postoperative spine scanning (c), the three-point Dixon technique (d) allows for more homogeneous fat suppression than with fat saturation, which improves the analysis of the surrounding soft tissues when looking for evidence of infection or fibrosis. Images courtesy of Sofia Brandão.
Fat suppression may be quite challenging whenever metallic materials are present. The fat-sat technique (a) may be replaced by short tau inversion recovery (STIR) (b) when the evaluation of the cartilage is not the main focus of the exam. In cases of postoperative spine scanning (c), the three-point Dixon technique (d) allows for more homogeneous fat suppression than with fat saturation, which improves the analysis of the surrounding soft tissues when looking for evidence of infection or fibrosis. Images courtesy of Sofia Brandão."General radiologists and radiographers, therefore, need to have extensive knowledge of the main applications and limitations of the pulse sequences included in their scanner's options. They should also be aware of the similarities between the sequences among the manufacturers, so they can adapt their own protocol from clinical or research papers," she said.
Despite real-time changes in the examination environment, she thinks it's important for operators to keep image quality optimal by applying their knowledge of pulse sequences to avoid artifacts during each study.
Speaking from experience, Brandão pointed to cardiac MRI, which relies on fast imaging and patient cooperation. Cine imaging is usually made with steady-state free precession (SSFP) pulse sequences, which are prone to susceptibility effects arising from lung-heart interfaces, or in patients with pleural effusion. The heterogeneity of the main field leads to local variations of the SSFP signal and dark-band artifacts.
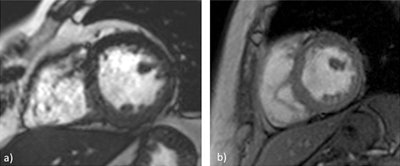 In cardiac imaging, steady-state free precession (SSFP) images (a) are quite useful for a dynamic evaluation of myocardial function. These sequences are prone to radiofrequency and magnetic field heterogeneities, and, therefore, they are sometimes replaced by spoiled gradient-recalled echo (GRE) images (b), despite the slight contrast decrease between the myocardium and the heart chambers. Images courtesy of Sofia Brandão.
In cardiac imaging, steady-state free precession (SSFP) images (a) are quite useful for a dynamic evaluation of myocardial function. These sequences are prone to radiofrequency and magnetic field heterogeneities, and, therefore, they are sometimes replaced by spoiled gradient-recalled echo (GRE) images (b), despite the slight contrast decrease between the myocardium and the heart chambers. Images courtesy of Sofia Brandão."There are possible solutions to this problem. These include ensuring the lowest possible repetition time, performing localized high-order shimming to reduce those steady-state signal dropouts, and performing the frequency scout to identify the frequency offset to further minimize these artifacts. That said, the use of spoiled gradient-recalled echo (GRE) sequences instead of SSFP may be the ultimate alternative to get good-quality images," she said.
Originally published in ECR Today on 7 March 2015.
Copyright © 2015 European Society of Radiology