Three clinical issues that may arise with theranostics treatments will require special provisions, including spot imaging, according to insights shared during the 124th annual meeting of the American Roentgen Ray Society (ARRS) in Boston.
Theranostics treatments are used with increasing frequency now since the approvals and expansions of Lutathera (lutetium-177 [Lu-177]) DOTATATE, a radiopharmaceutical for neuroendrocrine tumors (NETs) and Pluvicto, Lu-177 PSMA-617, for prostate cancer.
Though common but not serious side effects, sialoadenitis (inflammation of the salivary gland) and xerostomia (dry mouth) can occur with prostate-specific membrane antigen (PSMA) treatments. On the other hand, two serious side effects occurring less frequently are carcinoid crisis with DOTATATE therapies, and extravasations with any intravenous (IV) radiopharmaceutical therapies, explained Erica Cohen Major, DO, a nuclear medicine physician and assistant chief of nuclear medicine at Edward Hines VA Hospital near Chicago.
"We're seeing patients in rapid sequence, multiple times a week, maybe even multiple times a day; they're coming back every three to six weeks for labs, and we're having to make clinical decisions about things that we didn't even think about before," Major said.
Extravasations
Extravasations, in particular, are of interest to the U.S. Nuclear Regulatory Commission, Major noted, saying that risks of radiation injury to the skin from radioactive IV treatments could be significantly lower than medical literature implies, although more studies are needed especially as high-energy beta emitters and alpha emitters are increasingly used.
When a measurable amount of injectate leaks into subcutaneous tissues, this is called extravasation. It causes radiation injury that may be visible as dry desquamation or moist desquamation, for example. How much radiation will produce these findings can vary, but deterministic effect thresholds range from 2-15 gray (Gy), Major said.
The effects generally aren't seen until about one month after the incident has occurred.
"That's why it's important to pay attention to the patients and know at the time of administration that something has happened so we can be aware and counsel the patients and try to minimize the amount of radiation that's sitting in those subcutaneous tissues," Major said.
Major also shared an extravasation case study from 2020 of a 68-year-old female with a progressive midgut neuroendocrine tumor, who was administered 200 millicuries of lutetium DOTATOC. Immediately after the therapy was completed, the technologist noted there was swelling in the upper arm and suspected extravasation. Spot imaging revealed that more than half of the administered activity was in the patient's arm.
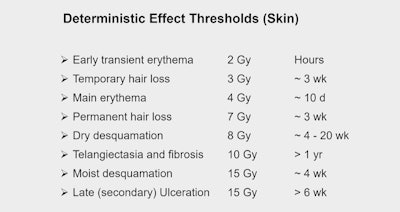 During an ARRS session on clinical issues encountered with radiopharmaeuticals, Erica Cohen-Major, DO, a nuclear medicine specialist at Edward Hines VA Hospital near Chicago shared gray (Gy) measures associated with extravasation-related radiation injury. (Graphic courtesy of Stephen Graves, PhD, University of Iowa)
During an ARRS session on clinical issues encountered with radiopharmaeuticals, Erica Cohen-Major, DO, a nuclear medicine specialist at Edward Hines VA Hospital near Chicago shared gray (Gy) measures associated with extravasation-related radiation injury. (Graphic courtesy of Stephen Graves, PhD, University of Iowa)
To protect the kidneys, the team doubled the patient's intake of amino acids over a 12-hour period (instead of 4 hours), and the patient was advised to elevate and exercise the arm, wrap it in a compression bandage, and use heated gel pads. Through repeat imaging a day later, it was estimated that only 1% of administered radioactivity remained in the patient's arm by that time, Major explained. In addition, dose calculations estimated mean dose to the arm of approximately 3 Gy. The patient spent a short time in the hospital but had no symptoms, and there were no complications in subsequent treatments or after during a one-year follow-up, Major added.
Serious radiation injuries seem to be a "rare occurrence," Major continued, adding that frequency might change now that more intravenous therapies are being used.
Other advice Major shared included considering advanced IV access if dealing with a difficult stick, always checking lines prior to injections, monitoring the injection site throughout the infusion, and considering routine spot imaging afterward to make sure there has not been an infiltration.
Carcinoid crisis
A dangerous event with DOTATATE treatments for NETs is carcinoid crisis, a sudden release of vasoactive substances into the bloodstream. Though rare, carcinoid crisis usually occurs within 48 hours after the first treatment. It can be life-threatening, Major said, and the nursing team may need to know what to do.
With the first treatment, observation for two days would be wise, especially in cases of high tumor burden in the liver. If carcinoid crisis is suspected, Major recommends turning off the infusion and giving doses of short-acting octreotide until symptoms are controlled.
In any event, consulting with oncology colleagues is key.
Trouble eating, dry mouth
More common but less dangerous with PSMA treatments are sialoadenitis and xerostomia. Major said imaging assessments are not needed for these conditions, but listening to patients will serve them well.
In one case, the power of a patient's favorite food alerted the nuclear medicine team to worsening symptoms. The patient had been regularly enjoying Chicago Portillo's Italian beef subs until he developed trouble eating them.
The clue was that the patient needed the sub fully soaked in broth or otherwise couldn't eat it, and he mentioned this to his care team. The sandwich became a new frame of reference, Major said.





















