CHICAGO - Evidence for the efficacy of whole-body FDG-PET/MRI continues to mount, as the hybrid modality outperformed MRI alone for staging women with suspected pelvic malignancies in a study presented at RSNA 2013 on Wednesday.
Researchers found that F-18 FDG PET/MRI correctly identified metastatic lesions and provided greater lesion conspicuity and diagnostic confidence than MRI alone.
"The added metabolic information of FDG-PET leads to a higher detection rate of lymph node and peritoneal metastases, as well as a higher diagnostic confidence in the differentiation of malignant or benign lesions," said lead author Dr. Karsten Beiderwellen from the department of diagnostic and interventional radiology and neuroradiology at University Hospital Essen.
During his presentation, he noted that previous studies have demonstrated FDG-PET/CT's accuracy for whole-body staging in gynecological cancer patients. Also, research has found MRI to be superior to CT for local tumor staging and restaging.
Initial retrospective studies using simultaneous PET/MRI in patients with pelvic malignancies have also shown promising results, he said.
Ovarian and cervical cancer
Beiderwellen and colleagues analyzed 20 patients with a mean age of 53 years (range, 25 to 72 years) who were suspected of having a recurrence of cervical or ovarian cancer. There were 10 cases of ovarian cancer and 10 cases of cervical cancer.
Among the patients, 18 underwent both whole-body PET/CT and PET/MRI (3-tesla Biograph mMR, Siemens Healthcare). Two patients received only PET/MRI scans for primary tumors.
The MRI protocol included T1-weighted pre- and postcontrast fat-saturated fast low-angle shot (FLASH); T2-weighted half-Fourier acquisition single-shot turbo spin-echo (HASTE); and diffusion-weighted imaging (DWI). PET scans were conducted for eight minutes per position with 228 MBq of FDG (± 45 MBq).
Two readers evaluated the datasets from FDG-PET/MRI, whole-body MRI, and whole-body MRI with DWI and rated each imaging technique's performance in terms of lesion conspicuity (on a four-point scale), lesion count and localization, lesion status (benign, malignant, or indeterminate), and diagnostic confidence (on a three-point scale).
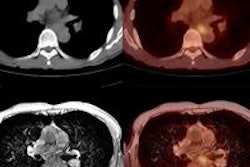
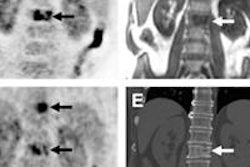
Image comparisons
Among the 20 patients, metastatic lesions were present in 17 women (85%). PET/MRI correctly identified all 17 patients, whereas MRI alone identified 15 (88%) of the 17 women.
"In these 15 patients, the malignant lesions were visible but could not be characterized as malignant [by MRI alone]," Beiderwellen said.
A total of 81 lesions were found: 61 malignant lesions and 20 benign. Again, FDG-PET/MRI correctly identified all malignant lesions, whereas MRI alone detected 55 (90%) of the 61 positive lesions. All lesions were visible on MRI, but the six remaining lesions were rated as "indeterminable."
FDG-PET/MRI achieved greater conspicuity for malignant lesions (3.9 out of 4.0, ± 0.3), compared with MRI alone (3.7 ± 0.6), according to the researchers. For benign lesions, FDG-PET/MRI had a conspicuity rating of 3.2 (± 1.1), compared with 3.1 (± 1.2) for MRI alone.
FDG-PET/MRI also showed greater diagnostic confidence for the detection of malignant lesions, with a median rating of 2.8 (out of 3.0, ± 0.4), compared with MRI alone at 2.2 (± 0.7). For benign lesions, FDG-PET/MRI had a diagnostic confidence of 2.2 (± 0.8), equal to that of MRI alone at 2.2 (± 0.9).
Based on the results, the researchers concluded that FDG-PET/MRI offer better detection of malignant lesions than MRI alone.
"Since PET/MRI leads to a higher diagnostic confidence, additional examinations might be avoided," Beiderwellen added.
He did cite some limitations to their research, including the small study cohort and the lack of histopathological correlation for all lesions.
Beiderwellen and colleagues next plan to compare the performance of PET/MRI with PET/CT for whole-body staging.