In most chest pain patients, coronary CT angiography (CTA) surpasses its rival -- stress myocardial perfusion scintigraphy (MPS) -- for diagnosing coronary artery disease, according to the results of a new model analysis comparing the two techniques.
In their model, Pennsylvania researchers found CTA-based diagnosis of chest pain to be cheaper, more accurate, and lower in radiation dose as long as disease prevalence in the patient population being studied remained less than 50%. The research begins to answer some of the questions regarding the point at which CTA becomes cheaper than nuclear stress testing, which has not been determined in previous studies.
Competing or complementary?
"Both coronary CTA and nuclear stress perfusion are used to evaluate coronary artery disease, and they can either be viewed as competing or complementary studies, because in some cases you can decide which test to do, and in some cases the two studies may combine to provide additional information," noted Dr. Ethan Halpern from Thomas Jefferson University in Philadelphia.
His group used a literature-based decision-tree analysis to find the optimal combination of coronary CTA and MPS to evaluate coronary artery disease, including diagnostic accuracy (false-positive and false-negative rates), imaging costs, and effective radiation exposure.
Clinicians are faced with a number of decisions regarding which imaging tool to use when a patient presents with possible coronary artery disease, Halpern said in a presentation at the 2009 RSNA annual meeting.
"You could study it with stress CT, or you could do CT followed by stress [MPS] if the CT was positive, or for the most part stress followed by CT," Halpern said. "In all of these cases, if all tests are positive you go to cardiac [catheterization], and if negative you go to medical therapy."
For stress MPS, Halpern and co-investigators including Anish Koka and Dr. David Levin used "well accepted" 88% sensitivity and 77% specificity levels in their model, Halpern said. By contrast, CTA sensitivity and specificity were somewhat conservative: 95% and 83%, respectively. Other specifications included:
- Radiation doses were pegged at 9.4-12.0 mSv for stress MPS, 4.2-10.0 mSv for coronary CTA, and 7-10 mSv for cardiac catheterization.
- Costs were based on the 2009 Medicare Physician Fee Schedule. In the model, diagnostic catheterization ($2,948) was performed only if coronary CTA ($662) and MPS ($681) studies performed were positive.
Although costs for coronary CTA and stress MPS are quite similar, the real driver of diagnostic costs is whether or not the patient is ultimately referred for catheterization, "because the cost of the cath is almost $3,000," Halpern said.
The researchers found that both imaging costs and effective radiation exposure rose linearly with the prevalence of coronary artery disease. Age, gender, and clinical presentation can be used to estimate the prevalence of flow-limiting coronary lesions in patients with suspected disease before they're scanned.
"At a prevalence below 50%, evaluation with coronary CTA reduces imaging costs and radiation doses relative to the standard technique," Halpern reported. Thus, he said, the reduced costs and dose with coronary CTA resulted from both CT's lower effective radiation dose and the reduced number of unnecessary cardiac catheterizations.
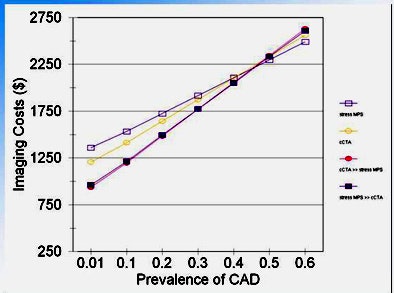 |
| Imaging costs, based on the 2009 Medicare Physician Fee Schedule, were nearly equivalent for both coronary CTA ($662) and MPS ($681), and overall costs were lower if diagnostic catheterization ($2,948) could be avoided. All images courtesy of Dr. Ethan Halpern. |
Using both tests -- coronary CTA plus stress MPS -- yielded slightly higher radiation exposures than coronary CTA alone, but costs were actually lower when both exams were used, due to the "marked decline in the cost of cardiac caths that we perform" in such a scenario, he said.
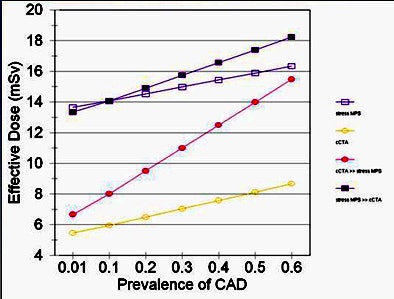 |
| Effective radiation dose (9.4-12.0 mSv for stress MPS, 4.2-10.0 mSv for coronary CTA, and 7-10 mSv for catheter-based angiography) rose linearly with the prevalence of coronary artery disease, and was lower for coronary CTA as long as disease prevalence remained less than 50%. |
Effective radiation "might also depend on what the odds are of a patient's getting a second study with radiation," Halpern said. The use of coronary CTA alone had the lowest effective dose -- so it remained even if a second (stress MPS) exam were needed, and even if ultralow-dose prospective gating techniques were not available for coronary CTA (leaving the dose at 10 mSv), he said.
"Even though you may still get a stress MPS study if you're positive [at CT], the dose is much lower, especially at a low prevalence, because CT is going to act as a gatekeeper that prevents you from getting the stress MPS test."
Finally, replacing stress MPS with coronary CTA reduced both false-positive and false-negative rates, Halpern said.
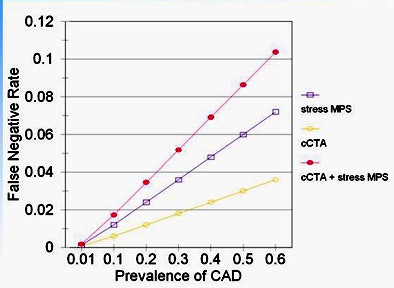
"If you use both tests, you slightly increase false negatives the way our algorithm works, because you require both studies to be positive before you say the patient can go on to catheterization," he said. "CT by itself has a lower false-negative rate than stress MPS."
As for the false-positive rate, it increases with disease prevalence for both exams, but remains lower for coronary CTA versus stress MPS across the board, and combining the exams reduces false-positives further, Halpern said.
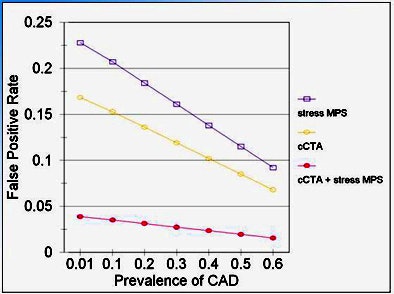 |
| The use of coronary CTA generally reduced levels of both false-positive (above) and false-negative (below) results compared to stress MPS. Combining the tests slightly increased the number of false negatives, because catheterization was not performed unless both were positive. |
 |
Both imaging costs and radiation dose are decreased by using coronary CTA for evaluating chest pain when the prevalence of flow-limiting coronary artery disease is below 50%, Halpern concluded. Using coronary CTA to evaluate chest pain in this population also reduced unnecessary cardiac catheterization procedures, radiation exposure, and the costs of workup.
The results mean that cost-effective utilization of coronary CTA should be guided by an assessment of clinical risk factors to ensure that the study population has an expected prevalence of less than 50% -- a level that can be calculated based on patient history and presentation, he said.
"Coronary CTA will result in a decline in catheterizations -- and we haven't even talked about the morbidity of those caths," Halpern said. Avoiding them "decreases morbidity for things like stroke."
By Eric Barnes
AuntMinnie.com staff writer
January 15, 2009
Related Reading
Patients with peripheral arterial disease may need cardiac imaging, December 30, 2009
Echocardiography test beats SPECT for predicting problems after MI, December 7, 2009
Echo plus ECG team up to find heart flaws in athletes, November 16, 2009
Routine cardiac stress testing not advised for young adults, August 10, 2009
Copyright © 2010 AuntMinnie.com