Gamma cameras that are equipped with a gadolinium-153 line source for attenuation correction can do double-duty as body outliners for localizing sentinel lymph nodes (SLN) prior to breast surgery, according to U.K. researchers.
The ability of gamma camera imaging to accurately pinpoint lymph nodes makes it a valuable tool for surgeons. Using a body-outline view insures such accuracy, wrote Elizabeth Clarke and colleagues from the City Hospital NHS Trust in Birmingham in the Journal of Nuclear Medicine. Clarke’s co-authors, Dr. Alp Notghi and Keith Harding, are also in the hospital’s department of physics and nuclear medicine.
"The aim of this study was to provide a technique that can achieve (a) body-outline view on both anterior and lateral projections," they wrote "The gamma camera images may identify SLNs at unsuspected areas...and may have a profound effect on the surgical approach," (JNM, September 2002, Vol. 43:9, pp. 1181-1183).
In order to determine the best method, three different body-outline techniques were tested. As a control, one patient was injected with 20-40 MBq of 99mTc-nanocolloid (Nanocoll, Amersham Health, Princeton, NJ) at four sites around the tumor. The woman then underwent surgery with a Navigator GPS probe (RMD Instruments, Watertown, MA) and blue dye for SLN detection.
In 24 patients, a manual body outline was conducted with the images acquired on a single-head Basicam camera (Siemens Medical Solutions, Hoffman Estates, IL). The camera was fitted with a general-purpose collimator. Two 300-second acquisitions were performed in the affected breast; the body outline was acquired by holding a 2 MBq 99m-Tc source and manually moving it around the affected breast and body. In one patient, a 57Co flood was used to obtain the body outline.
In 25 patients, a 153Gd line source on a Prism 2000 gamma camera (Philips Medical Systems, Andover, MA) was used to acquire the body outline. Transmission and emission images were acquired simultaneously with a 99mTc window (140 keV) and a 153Gd window (159 KeV), the authors stated. Emission images were acquired for 300-seconds; transmission images were acquired at 120 seconds in both anterior and lateral projections.
As for the surgeons’ preferences, they found that using the 153Gd line-source method resulted in good-quality body-outline images for anterior and lateral views. In this group of patients, body-outline imaging targeted 73% of the sentinel lymph nodes; 96% of the SLN were found using the probe and 68% with blue dye. Using the 153Gd line-source method, the mean localization and resection time was 14 minutes, the paper stated.
The manual body-outline method and the 57Co flood technique produced low-quality images; the surgeons were dissatisfied with the results because only an anterior transmission view was possible, the group wrote.
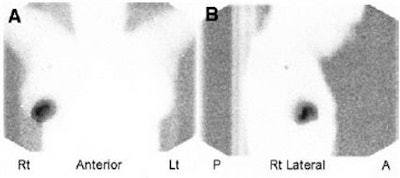 |
| Sentinel lymph node images acquired on a dual-head gamma camera with 153Gd line-source transmission. On the right is the anterior view; on the left the posterior view. Images courtesy of Elizabeth Clarke and the Journal of Nuclear Medicine |
"A 153Gd line source gives a clear, crisp body-outline image," the authors concluded. "This technique also gives a low radiation dose to the patient and none to the operator. The extra radiation dose to the patient from the 153Gd source is 3 m Sv per (2) views, 1% of the total patient dose from the SLN study." More conveniently, this method can be performed on most dual-head gamma cameras with attenuation-correction capability.
Other investigators have had similar success with body-outline techniques. A group from Keio University School of Medicine in Tokyo used lymphoscintigraphy with scattered photons to create their outline. In this case, lymphoscintigraphy was performed 3-4 hours after the injection of 111 MBq of 99mTc tin colloid into the peritumoral region. Images were obtained with dual-energy windows of 130-150 keV for the primary photons and 70-110 keV for the scattered photons.
"The images constructed from the scattered photons clearly showed the contours of the body, and the fusion images constructed from the primary and scattered photons allowed for easy identification of the location of the sentinel nodes," the researchers reported (Annals of Nuclear Medicine, October 2000, Vol. 14:5, pp. 401-404).
By Shalmali PalAuntMinnie.com staff writer
October 21, 2002
Related Reading
New camera may improve scintimammography, August 6, 2002
Scintigraphy predicts response to doxorubicin in advanced breast cancer, August 6, 2002
Radiodetection may find more than one sentinel node, June 17, 2002
Scintimammography catches chemoresistance in breast cancer patients, June 13, 2002
Copyright © 2002 AuntMinnie.com