CHICAGO – Gallium-68 (Ga-68) RM2-PET/MRI is better than MRI alone for detecting relapse in prostate cancer patients, according to research presented November 26 at RSNA 2023.
Moreover, the approach could help detect disease that other effective prostate cancer PET radiotracers may miss, said Heying Duan, MD, a nuclear medicine research scientist at Stanford University, during a November 26 scientific session.
“You've hear a lot about PSMA. I wanted to introduce a new player in the game: gallium-68 GRPR antagonist,” Duan told attendees, during a scientific session on prostate cancer imaging.
Several prostate-specific membrane antigen (PSMA) PET radiotracers for detecting BCR prostate cancer have been approved in the U.S., such as Ga-68 PSMA-11 and F-18 DCFPyl (Pylarify, Lantheus Medical Imaging) and are included in National Comprehensive Cancer Network guidelines, Duan explained. Yet up to 10% of cases do not express PSMA, she noted.
Thus, Duan and colleagues developed a tracer called Ga-68 RM2, which targets other receptors overexpressed in prostate cancer – namely, gastrin-releasing peptide receptors (GRPRs). Previous studies by the team found the tracer is effective at revealing this activity on PET.
In her presentation, Duan presented a final analysis of a recently completed phase II/III imaging trial of Ga-68 RM2-PET/MRI compared with MRI alone in patients with biochemically recurrent (BCR) prostate cancer.
Out of 209 patients screened between December 12, 2015 and July 27, 2021, the researchers included 100 patients. Patients were eligible if they were older than 18 and had rising blood levels of PSA ( ≥ 0.2 ng/mL after prostatectomy or ≥ 2 ng/mL after radiotherapy) and negative conventional imaging (CT and/or bone scans).
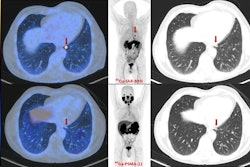
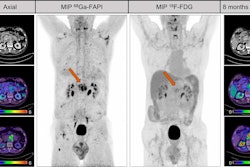
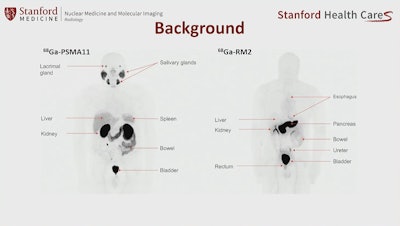 An image showing potentially different sites of PET radiotracer uptake by prostate cancer tumors between U.S. approved Ga-68 PSMA-PET and experimental Ga-68 RM2. Image courtesy of Heying Duan, MD, Stanford University.
An image showing potentially different sites of PET radiotracer uptake by prostate cancer tumors between U.S. approved Ga-68 PSMA-PET and experimental Ga-68 RM2. Image courtesy of Heying Duan, MD, Stanford University.
The primary endpoint was the diagnostic performance of Ga-68 RM2-PET/MRI versus MRI alone, with the imaging sets interpreted by three independent experts using a standardized evaluation criteria.
Ga-68 RM2-PET/MRI showed significantly higher detection rates than MRI alone (143 versus 96 lesions). In addition, the sensitivity of Ga-68 RM2-PET/MRI was higher than MRI alone (85.2% vs. 49.4%) and specificity was comparably high (100% vs. 94.7%), according to the findings.
“The collective findings of this comparative imaging trial and other published studies provide compelling evidence that Ga-68 RM2-PET/MRI not only outperforms conventional imaging with MRI but also shows higher reliability and number of lesions detected, which could potentially affect subsequent patient management,” Duan noted.
Ultimately, given high intratumor heterogeneity in prostate cancer, targeting a single tumor characteristic might not be sufficient to reflect the full extent of disease, Duan noted. Therefore, Ga-68 RM2-PET should be considered in addition to PSMA-PET in BCR prostate cancer patients to aid in disease detection and management decision, she suggested.
Nonetheless, further prospective comparative studies with PSMA-targeted PET are needed to gain a better understanding of GRPR and PSMA expression patterns in the disease, Duan concluded.
“GRPR-targeted PET imaging is a valuable tool in the imaging armamentarium of prostate cancer at biochemical recurrence,” Duan concluded.
Duan received a Trainee Research Prize for fellows for the work.