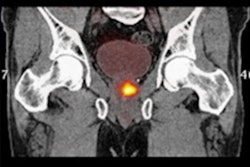
Prostate-specific membrane antigen (PSMA)-PET imaging with a gallium-68 PSMA-11 radiopharmaceutical may save a significant number of prostate cancer patients from surgery, according to authors of a research letter published September 12 in JAMA Network Open.
A team of U.S. researchers applied a validated risk calculator to quantify the association of routine PSMA-PET use with tumor upstaging in a large group of high-risk prostate patients who had undergone surgery. Over a seven-year period, they found a 16.3% median risk of upstaging from PSMA-PET imaging within the entire cohort.
"The risk of upstaging has steadily increased over time, a trend that may be secondary to higher proportions of Gleason grade group 4 and 5 cancers being found after surgery," wrote corresponding author Dr. Jonathan Shoag of Case Western Reserve University in Cleveland, OH, and colleagues.
Ga-68 PSMA-11 was the first PET imaging radiotracer approved by the U.S. Food and Drug Administration for diagnosing PSMA-positive lesions in men with prostate cancer. The radiotracer has been proven to detect more nodal and metastatic disease compared with conventional imaging in patients after surgery, and it has been added to National Comprehensive Cancer Network (NCCN) guidelines for imaging prostate cancer.
Current evidence and guidelines recommend radiation therapy with androgen deprivation therapy as the preferred treatment over invasive surgery for prostate cancer with node-positive disease detected by conventional imaging.
"However, it is unknown whether men with positive nodes detectable by PSMA-PET but undetectable by conventional imaging benefit preferentially from radiotherapy," the authors wrote.
Thus, in this study, the researchers applied what they have named the "UCLA PSMA Risk Calculator," a validated nomogram for calculating the likelihood of upstaging on Ga-68 PSMA-PET, in patients listed in the National Cancer Database (NCDB) who underwent radical prostatectomy from 2010 to 2017.
All patients were identified as having clinically localized high-risk disease. The authors culled data on 352,521 patients and deemed a total of 45,772 individuals eligible for the study after exclusions, such as missing Gleason grade scores, PSA levels, or biopsy core data.
According to the findings, the median risk of PSMA-PET upstaging across the entire cohort was 16.3% from 2010 to 2017, and it increased year by year, from 13% in 2010 to 17.6% in 2017. In addition, both nodal and distant metastatic risk for upstaging significantly increased over time, from 11.7% in 2010 to 15.4% in 2017 (p < 0.001) and from 3.6% in 2010 to 4.7% in 2017.
"While upstaging may be secondary to nodal or distant metastatic findings on PSMA-PET, the risk of nodal upstaging in particular may affect the decision between surgery and radiation," the authors wrote.
The researchers noted that limitations exist in the true predictive accuracy of the risk calculator itself, given that previous work has estimated its receiver operative curve at 0.74. Nonetheless, wider use of PSMA-PET may result in more patients being found with occult nodal or metastatic disease, they suggested.
"The immediate impact of stage migration from PSMA PET may be to alter treatment decisions in a substantial number of patients with high-risk prostate cancer," Shoag and colleagues concluded.