FDG-PET scans showed patients taking lipophilic statins may have more than double the risk of converting to dementia over eight years of follow-up compared with those not taking statins, according to a presentation on June 14 at the Society of Nuclear Medicine and Molecular Imaging (SNMMI) meeting.
Researchers analyzed PET imaging of patients enrolled in the national Alzheimer's Disease Neuroimaging Initiative (ADNI) who were taking a lipophilic statin for high cholesterol and found that they had a substantial decline in metabolism in the posterior cingulate cortex area of the brain compared with patients who were taking other statins or none at all. Posterior cingulate hypometabolism is associated with early Alzheimer's disease.
"We are providing a new application of PET to further our understanding of the relationship between one of the most commonly used classes of drugs and one of the most common afflictions of the aging brain," said lead study author Prasanna Padmanabham of the University of California, Los Angeles, in a statement released by the SNMMI.
Overwhelming evidence supports the use of statins to reduce low-density lipoprotein cholesterol (LDL-c) to reduce the risk of heart attacks and stroke. Studies suggest lipophilic statins may carry a higher risk for patients because of their increased ability to cross the blood-brain barrier, although a direct link between cognitive decline and the medication has not been proved.
In fact, studies of the relationship between the use of statins (HMG-CoA reductase inhibitors) and subsequent cognitive performance have been variously reported to demonstrate beneficial, harmful, or no significant effects, according to the researchers.
In this study, the researchers sought to help clarify the relationship between statin use and patients' long-term cognitive trajectory by analyzing FDG-PET scans. They compared users of statins that are known to have moderate (atorvastatin) or high (simvastatin) lipophilicity and blood-brain barrier penetration to people who didn't use statins or those who used other statins.
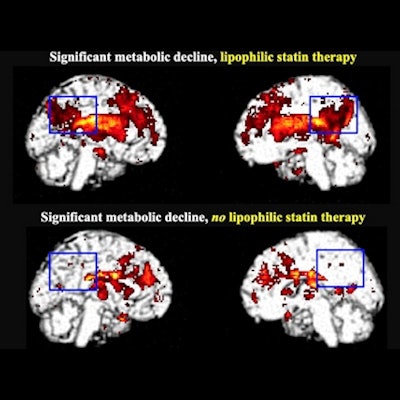
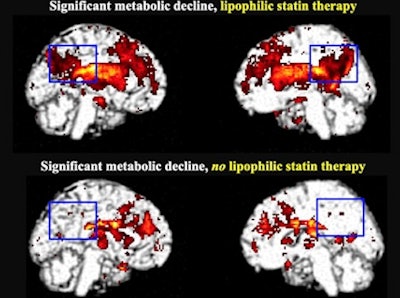 Significant metabolic decline in the posterior cingulate cortex in lipophilic statin users after five to six years (top) compared with hydrophilic statin users and those not taking statins (bottom). Image courtesy of Prasanna Padmanabham.
Significant metabolic decline in the posterior cingulate cortex in lipophilic statin users after five to six years (top) compared with hydrophilic statin users and those not taking statins (bottom). Image courtesy of Prasanna Padmanabham.Out of 392 patients with mild cognitive impairment, researchers included 303 who had cholesterol levels available at baseline. Participants were split into groups based on three parameters: baseline cognitive status, baseline cholesterol levels, and type of statin used. Participants underwent FDG-PET imaging to identify any regions of declining cerebral metabolism within each statin group. Eight years of subject clinical data were analyzed.
Over a follow-up period of 96 months, 24% of the lipophilic statin group converted to dementia compared with 10% of patients who were not taking statins. The conversion rate of people taking other statins did not significantly differ from patients not taking the medication. In addition, posterior cingulate metabolic decline was identified among lipophilic statin users, while no significant decline occurred among the other groups.
"Among subjects with early mild cognitive impairment and low to moderate serum cholesterol levels at baseline, lipophilic statin use was associated with more than double the risk of converting to dementia over eight years of follow-up compared with statin nonuse," Padmanabham said.
The researchers concluded by suggesting the findings could be used to inform a patient's decisions regarding which statin may be most optimal to use while preserving their cognition and ability to function independently.