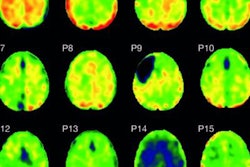
A novel PET imaging technique has uncovered high levels of ischemia in patients within the first 24 hours after a traumatic brain injury (TBI), but it also showed the condition does begin to subside over the next 10 days, according to a study published online November 11 in JAMA Neurology.
European researchers used oxygen-15 (O-15) PET to measure cerebral blood flow, oxygenation, ischemic brain volume, and other related factors in nearly 70 patients with TBI and came away with three key findings, one of which is O-15 PET's utility to detect ischemia soon after a TBI.
"Second, [the results] elucidate the association between cerebral blood volume increases and intracranial hypertension and the relevance of this association for intracranial pressure management," wrote the authors, led by Yoann Launey, PhD, from the University of Cambridge in the U.K. "Finally, these data document abnormal flow-metabolism coupling and cerebral vasoregulation after TBI, which is a potential target for the development of future therapeutic interventions."
Beyond the obvious initial adverse effects of TBI, the injury can lead to ischemia, brain swelling, and intracranial hypertension. In such cases, it is critical that adequate cerebral blood flow be maintained to carry oxygen throughout the brain. While O-15 PET is the current standard to measure cerebral blood flow, cerebral oxygen metabolism, and oxygen extraction fraction -- all of which are used to measure ischemia -- previous research has been "hampered by differences in PET methodology and approaches to data analysis," the study authors wrote. "There remains a need for comprehensive characterization of cerebrovascular physiology after TBI using standardized O-15 PET in a large patient sample across the full temporal disease narrative."
To that end, Launey and colleagues retrospectively looked at 68 patients (mean age, 29 years; range 22-47 years) with TBI who required intracranial pressure monitoring. These patients underwent a total of 90 O-15 PET scans, of which 17 studies (19%) were performed on the first day of their injury, 54 exams (60%) were conducted two to five days later, and 19 scans were done six to 10 days later. Those results were compared with scans from 20 healthy control subjects (mean age, 43 years; range 31-47 years).
Along with assessing cerebral blood flow and cerebral oxygen metabolism, the researchers also compared ischemic brain volume with jugular venous saturation and brain tissue oximetry, which combined is a measurement of brain oxygenation.
The researchers observed significantly less global cerebral blood flow and cerebral oxygen metabolism among TBI patients, compared with healthy controls. The same trend was apparent in regard to ischemic brain volume in comparison of the two groups.
| O-15 PET results during first 24 hours after TBI | |||
| TBI patients | Healthy controls | p-value* | |
| Cerebral blood flow | 26 mL/100 mL/min | 38 mL/100 mL/min | < 0.001 |
| Cerebral oxygen metabolism | 62 µmol/100 mL/min | 131 µmol/100 mL/min | < 0.001 |
| Ischemic brain volume | |||
| Within 24 hours of TBI | 36 mL | 1 mL | < 0.001 |
| 6-10 days after TBI | 24 mL | 1 mL | < 0.001 |
*Results are statistically significant.
In addition, cerebral blood flow reduction was at its peak during the first 24 hours and showed a trend toward high oxygen extraction fraction, which are classic indications of ischemia. Coincidentally, ischemic brain volume was at its highest less than 24 hours after TBI, compared with healthy controls, with many patients still presenting with increases in ischemic brain volume, albeit lower, six to 10 days after the brain injury.
Launey and colleagues found the presence of ischemia in the first 24 hours in approximately two-thirds of patients, and ischemia "is detectable up to 10 days postinjury and is not limited to patients with intracranial hypertension," they wrote. "We found significant outcome associations with ischemia that occurred early but not after 24 hours, implying that other pathophysiological mechanisms of energy failure may be dominant during later phases of the disease narrative."