Patients with bulimia nervosa may be more vulnerable to redeveloping the disorder, or even other eating disorders, because of changes in the brain’s serotonin levels, according to researchers from the University of Pittsburgh School of Medicine.
Dr. Walter Kaye, professor of psychiatry, and Dr. Guido Frank, visiting instructor in the department of psychiatry, used PET to image the brains of two study groups, consisting of 21 women in total. Nine previously had bulimia and maintained recovery for more than a year, and 12 were healthy with no history of eating disorders. The findings are presented in the latest issue of the American Journal of Psychiatry.
PET imaging was performed with the radioligand [18F]altanserin, a specific 5-HT2A receptor antagonist, on an HR+ scanner (Siemens Medical Systems, Hoffman Estates, IL). Scans were done during the first 10 days of the follicular phase for all subjects. In addition, MRI images were acquired and then aligned to the PET exams.
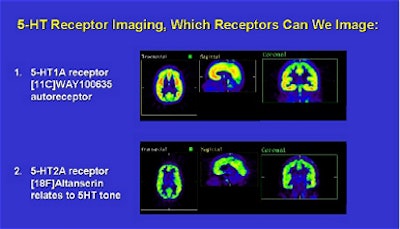 |
The image data showed that healthy women experienced an age-related decline in serotonin binding, while recovered bulimics did not.
"These data confirm and extend the possibility that a disturbance of serotonin neuronal activity is present after recovery from bulimia nervosa. The women who never had bulimia had an age-related decline in serotonin binding, but binding was not associated with age in the women who had recovered from bulimia nervosa," the authors wrote (American Journal of Psychiatry, July 2001, Vol. 158:7, pp. 1152-1155).
The researchers also found that women who recovered from bulimia had a "significantly lower level" of serotonin binding in the medial orbital frontal cortex (t=2.7, df=19, p=0.02) than the group of nonbulimic women. Moreover, the images of the recovered bulimics showed a "nonsignificant lower level" in the lateral orbital frontal cortex (t=1.7, df=13.8, p=0.09) and sensorimotor cortex (t=1.8, df=13.4, p=0.09), according to the study.
 |
Kaye said the findings confirm that biological factors may contribute to the pathogenesis of bulimia nervosa. The impulsive and compulsive behaviors commonly associated with bulimia nervosa may be due to the disturbance of the serotonergic system, he added.
"The images support the possibility that these alterations may be related to the control of appetite, mood, and impulse control, and thus may make some women vulnerable for developing an eating disorder. Moreover, the fact that serotonin activity did not normally change with age offers important clues as to why bulimia nervosa may develop in teenage years," he wrote.
The next phase of research will include a larger study group to verify the current findings, Kaye wrote.
Other researchers have reached similar conclusions. Psychiatrists from the University of Vienna relied on SPECT imaging to track the pathophysiology of bulimia nervosa. Using a different radiotracer ([123I]-2beta-carbomethoxy-3beta-(4-iodophenyl)tropane ([123I] beta-CIT), the group found that drug-free bulimia nervosa patients showed a 17% reduced brain serotonin transporter availability in the hypothalamus and thalamus and a similar reduction in striatal dopamine transporter availability (Biological Psychiatry, February 15, 2001, Vol.49:4, pp. 326-332).
And at the department of psychosomatic medicine at Kagoshima University Hospital in Japan, investigators used SPECT to characterize regional cerebral blood flow patterns in anorexia nervosa patients with binge/purge patterns. SPECT was performed before and after the subjects were asked to imagine food. The patients with habitual binge/purge behavior had significantly higher blood-flow percentage changes in the inferior, superior, prefrontal, and parietal regions of the right brain, they concluded (American Journal of Psychiatry, September 2000, Vol.157:9, pp. 1520-1522).
By Jennifer LungAuntMinnie.com staff writer
July 20, 2001
Copyright © 2001 AuntMinnie.com




















