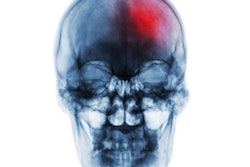
Faster intervention with endovascular thrombectomy for large vessel occlusion (LVO) stroke improves patient-reported quality of life outcomes, according to an article published June 3 in JAMA Neurology.
An international team of researchers studied patient answers to quality-of-life questions given during follow-up visits up to three months after undergoing the procedure and found that those who had faster “door-to-puncture times” reported greater improvements.
“Faster treatment with endovascular thrombectomy was associated with a substantial improvement in outcomes from the perspective of the patient,” noted lead author Raed Joundi, MD, PhD, of McMaster University in Hamilton, Ontario, Canada.
Endovascular thrombectomy (EVT) is a highly effective imaging-guided therapy in acute ischemic stroke with large vessel occlusion. The procedure is performed by interventional radiologists and its effect is highly time-dependent, whereby faster treatment from stroke onset improves reperfusion and clinical outcomes, the authors explained.
They noted that demonstrating an association between time to treatment and patient-reported quality of life may provide further impetus for quality improvement initiatives for stroke workflow using patient-reported outcome measures.
“It is fundamentally important to consider the patient’s perspective when implementing interventions or systems changes,” the group wrote.
To that end, the researchers analyzed in-person responses to quality-of-life questions given at 30 and 90 days during follow-up visits by patients who participated in a study testing the efficacy of EVT in a previous trial. The trial was conducted between March 2017 and August 2019 with patients recruited from seven countries.
Out of 1,105 patients who participated, there were 896 survivors with complete questionnaire scores at 90 days. The researchers split the patients into 15-minute cohorts based on how quickly they underwent the procedure from the time they arrived at the hospital. The median door-to-puncture time among the group was 59 (42-84) minutes, and half of the patients received EVT within 60 minutes.
According to a statistical analysis, every 15 minutes of faster door-to-puncture time was associated with a higher reported probability of “no or slight problems” in each of five domains: mobility (2.8%), self-care (2.2%), usual activities (2.6%), pain or discomfort (1.9%), and anxiety or depression (2.7%).
“We found a strong and consistent association between speed of treatment with EVT from hospital arrival and patient reported health-related quality of life at 90 days after acute ischemic stroke,” the researchers wrote.
Ultimately, the findings emphasize that programs and systems to shorten treatment times to EVT are critical, the authors noted. Potential opportunities for improvements include prenotification tools, automated LVO detection tools, preprepared EVT kits, availability of around-the-clock neurointerventional teams, and transferring patients directly from brain imaging suites to angiography suites, they suggested.
“These results support the beneficial impact of door-to-treatment speed on patient-reported outcomes and should encourage efforts to improve patient-centered care in acute stroke by optimizing in-hospital processes and workflows,” the authors wrote.
The full study is available here.