An AI model trained on chest x-rays shows promise as a noninvasive screening tool for achalasia, according to a study published September 18 in Clinical Gastroenterology and Hepatology.
With few noninvasive tests available for diagnosing the swallowing condition, the AI model could enable earlier diagnosis, noted corresponding author Akinari Sawada, MD, PhD, of Osaka Metropolitan University in Japan, and colleagues.
“In Japan, chest x-rays are commonly taken during regular health checkups. Based on the findings of this study, it may be possible to screen for esophageal achalasia in a simple and minimally invasive manner,” Sawada said in a news release from the university.
Achalasia is a rare progressive disorder that results from damage to nerves in the esophagus, which prevents the esophagus from squeezing food into the stomach. Symptoms include a backflow of food in the throat (regurgitation), chest pain, and weight loss, the authors explained.
Established tests for achalasia include high-resolution manometry, esophagogastroduodenoscopy, and barium swallow tests. Alternatively, plain chest x-rays can capture several characteristic signs of the condition, such as air-fluid level, opacity, and air esophagogram around the mediastinum, the researchers noted.
To explore whether an AI model could be a useful screening tool for the condition, the group trained a deep-learning AI model using 207 chest x-rays from 144 patients with esophageal achalasia and 240 chest x-rays from age- and sex-matched individuals without it. The diagnostic capability of the AI model was then verified using a test dataset consisting of 17 chest x-rays from 17 patients with esophageal achalasia and 64 chest x-rays from patients without.
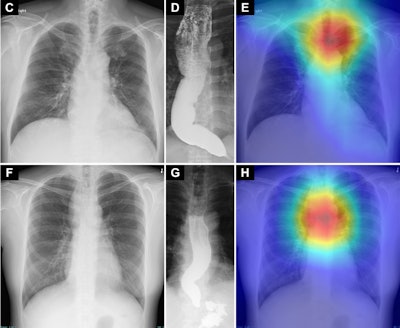 Saliency maps using Grad-CAM++ (E and H) show the model’s point of interest in chest radiographs (C and F) of patients with achalasia. The model’s point of interest is highlighted with red, yellow, and green. In both the upper and lower panels (E and H), the point of interest is located in a region around the upper esophagus that corresponds to an air esophagogram and/or air-fluid level in the esophagus in the barium esophagogram (D and G). Osaka Metropolitan University. Image available for republishing under Creative Commons license (CC BY-NC-ND 4.0)
Saliency maps using Grad-CAM++ (E and H) show the model’s point of interest in chest radiographs (C and F) of patients with achalasia. The model’s point of interest is highlighted with red, yellow, and green. In both the upper and lower panels (E and H), the point of interest is located in a region around the upper esophagus that corresponds to an air esophagogram and/or air-fluid level in the esophagus in the barium esophagogram (D and G). Osaka Metropolitan University. Image available for republishing under Creative Commons license (CC BY-NC-ND 4.0)
“There are reports indicating that from the onset of symptoms to diagnosis, esophageal achalasia takes an average of 6.5 years," Sawada said. "Delayed diagnosis may worsen esophageal dilation and tortuosity and reduce treatment efficacy; therefore, early diagnosis is desirable."
To that end, the AI model developed in this study may be a novel and promising noninvasive screening tool, the researchers concluded.
The full study is available here.