A simple technique that provides three-point support for scoliosis patients during slot-scanning digital radiography works well for evaluating them prior to spinal fusion surgery, according to Singaporean clinicians who illustrated the method June 1 in the European Journal of Radiology.
The researchers reported that giving patients a four-legged walking stick to hold and providing a cushion for them to rest their heads on during slot-scanning digital radiography (SSDR) helps them hold still and achieve maximum bending positions, which could prevent surgical spinal fusions that are longer than necessary.
"We have found this technique easy to learn and apply, with high reproducibility," wrote senior author Dr. Kevin Lim, chair of surgery at KK Women's and Children's Hospital in Singapore.
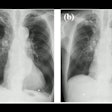
Assessing spinal flexibility in patients with severe, progressive scoliosis is necessary prior to spinal fusion surgery to preserve the maximum number of a patient's mobile spinal segments. Slot-scanning digital radiography (SSDR) provides images equivalent to supine side bending with about one-fifth of the radiation dose.
SSDR is increasingly available around the world and is the preferred modality for upright, erect scoliosis imaging, yet the practice of acquiring side-bending radiographs in the standing position using SSRD is not well-established, and limitations remain in the patient's ability to hold still during the procedure, according to the authors.
Lim and colleagues described and illustrated a simple technique they are using at their hospital to overcome these limitations.
The technique requires two height adjustable positioning aids: a four-legged walking stick for patients to hold on to and a triangular sponge for them to rest their heads on at the position of maximal bend. The triangular sponge is taped to the wall and covered with a disposable surgical cap which can be quickly replaced for the next patient.
Right side-bending radiographs are acquired posteroanterior with the patient facing the scanner. Patients are asked to bend to the right to bring their head and neck as close to the 3 o'clock position as possible.
At maximal bend, the patient's left arm is raised overhead to touch the opposite side of the cubicle for support. To maintain this extreme bend, the patient rests their head on the triangular sponge and holds on to the quad stick with their right hand, which aligns their head and trunk in one plane with shoulders and hips facing squarely forward.
Left side-bending radiographs are acquired anteroposterior with the patient's back against the detector. The patient is asked to bend to the left to bring their head and neck as close to the 9 o'clock position as possible. At maximal bend, the patient's right arm is raised overhead to touch the opposite side of the cubicle for support, which aligns their head and trunk in one plane with shoulders and hips facing squarely forward. The patient holds the quad stick with their left hand while their head rests on the sponge.
 Maximal side bend in acquiring an anteroposterior left-bending radiograph. Image courtesy of the European Journal of Radiology
Maximal side bend in acquiring an anteroposterior left-bending radiograph. Image courtesy of the European Journal of Radiology"With the use of simple positioning aids and three-point support to increase stability, the degree of side bending on standing radiographs acquired using SSDR have been excellent," the authors reported.
For both right and left side-bending imaging, the level of the sponge and height of the quad stick are applied at an appropriate level by the radiographer. The authors noted that they remind patients of the importance of side-bending radiographs for selection of surgical fusion levels and ask them to perform five to 10 right and left side-bending stretches to prepare for the x-rays. Begin the study with the side the patient can bend better toward, they suggested.
"We believe this will be the new gold standard for side-bending radiographs in scoliosis," the researchers concluded.