Imaging and clinical features of interstitial lung abnormalities (ILA) can predict progression to idiopathic pulmonary fibrosis (IPF), according to research presented February 26 at ECR in Vienna.
Tracking these features could improve patient care, according to a team led by presenter Tician Schnitzler, MD, of the University of California, San Francisco.
"[Our] findings could improve risk stratification, guiding timely monitoring and interventions to enhance patient outcomes," he and colleagues noted.
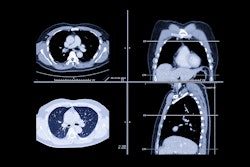
ILA is a common incidental finding on CT, and indicates early or mild fibrosis, the researchers explained. Although most ILA cases do not progress, some advance to IPF, leading to severe outcomes. That's why accurately assessing the severity of ILA on noncontrast chest CT is key to guiding patient follow-up and determining best treatment.
Schnitzler and colleagues conducted a study to identify imaging and clinical features on CT that could predict a patient's progression from ILA to IPF. The research included 746 patients from a longitudinal interstitial lung disease database; of these, 525 made up a low-risk ILA cohort and 221 made up a high-risk cohort. The investigators analyzed the following imaging features: subpleural fibrotic reticulation, cranial extent of fibrosis, anterior lung involvement, and emphysema severity; they incorporated the clinical variables of age and gender.
The group found the following:
| Comparison of CT findings among individuals at low- and high-risk interstitial lung abnormalities | |||
|---|---|---|---|
| Measure | Low-risk ILA cohort | High-risk ILA cohort | p-value |
| Subpleural fibrotic changes | 36% | 78% | < 0.001 |
| Cranial extent of fibrosis | 14% | 61% | < 0.001 |
| Anterior lung involvement | 37% | 86% | < 0.001 |
| Severe emphysema | 39% | 48% | < 0.001 |
It also reported that the high-risk ILA cohort was older compared with the low-risk group, with a mean age of 73 years compared with 71 years. There was no significant gender difference.
The investigators suggested that "future research should validate these findings in larger, multicenter cohorts."
In a related study presented in the same session, Schnitzler reported on study findings that showed that almost half of lung cancer cases in ILD had delayed diagnoses, with an average delay of 3.4 years -- although he and colleagues did not discover significant difference in mortality between early and delayed detection cases.
Patients with ILD are at increased risk of lung cancer, but finding the disease can be tricky due to background fibrosis – which can then lead to diagnostic delays, the group explained. Since research on lung cancer in ILD is scarce, the investigators conducted a study that analyzed delayed lung cancer diagnoses in ILD patients, tracking tumor stage at diagnosis, growth rates, treatment regimens, and outcomes.
Their study included 77 patients with concurrent ILD and lung cancer. A thoracic radiologist reviewed chest CTs for the following: earliest visible and reportable lesion time, when a lesion was first deemed suspicious, and the lesion's growth rate; the team also analyzed tumor staging, treatment regimens, and outcomes.
Schnitzler's group found that in 47% of the 77 cases, diagnosis was delayed, with an average delay of 3.4 years. These diagnostically delayed cases had a mean annual growth rate of 293% and a mean doubling time of 3.3 years, according to the team, which also noted that median patient survival time was 1,269 days for cancers that were found early compared with a median patient survival time of 867 days for cancers that were diagnostically delayed -- although this difference was not statistically significant.
For more coverage from ECR 2025, visit our RADcast on AuntMinnieEurope.